Objectives of the Guide
The objectives of Occupational Health and Safety: A Guide for ONA Members are to:
- Provide ONA members with a basic understanding of occupational health and safety law and principles and how they apply to health-care workplaces.
- Empower members with measures they can take, through the rights given to them under the Occupational Health and Safety Act, for the prevention of injuries and the elimination of the hazards in our workplaces.
- Encourage ONA occupational health and safety representatives to take more active roles in promoting health and safety initiatives in their Bargaining Units.
- Provide ONA members with valuable tools and resources to help them deal with occupational health and safety issues and make their workplaces safe and healthy.
Although this guide is very detailed, the information contained is not exhaustive and is intended only to provide general guidance and information about WSIB claims.
How to use this guide:
- Section I: The Internal Responsibility System
- Section II: The Law
- Section III: Hazardous Conditions & Substances
- Section IV: Education and Training
- Section V: Make it work for you
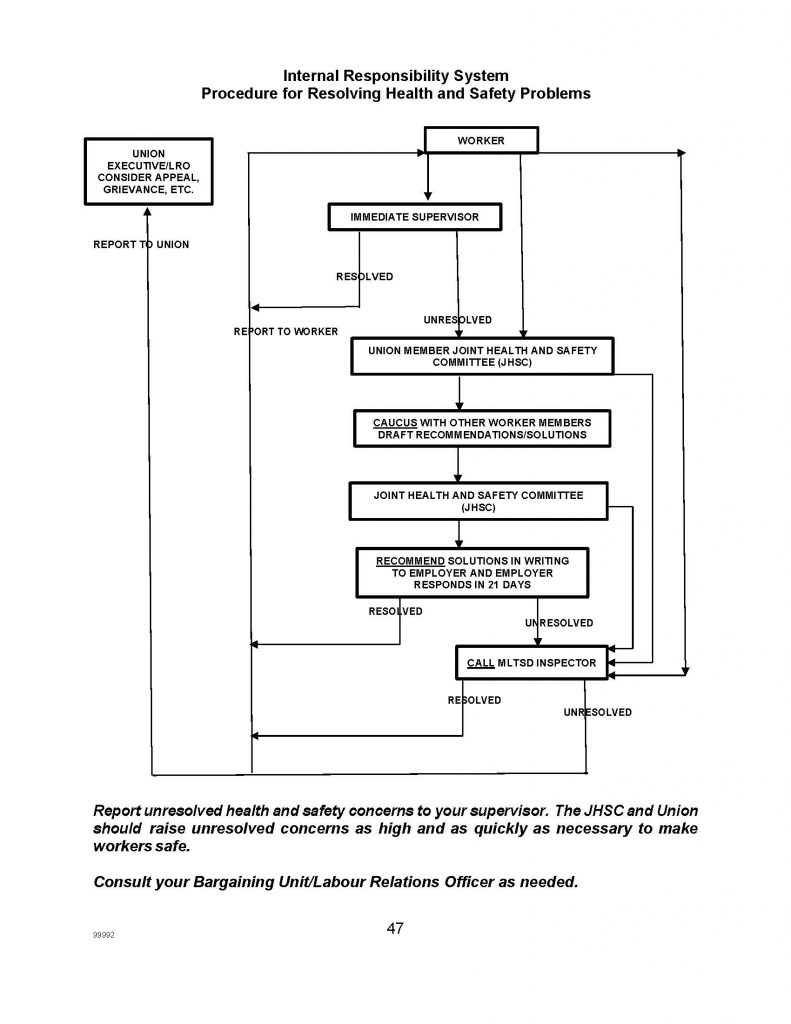
- Resolving health & safety problems
- Sample Scenarios
- Appendix A
- Appendix B
- Appendix C
- Appendix D, E, F
- Appendix G
- Appendix H
- Appendix I
- Appendix J
Occupational Health and Safety and the Internal Responsibility System
Occupational Health and Safety in the Health-care Sector
ONA has battled health and safety problems in health-care facilities for many years. Violence, needlestick injuries, musculoskeletal disorders also known as repetitive strain injuries (RSIs) and exposure to infectious diseases are just some of the health and safety hazards our members face daily and that generate continuously high injury rates in the health-care sector. Speaking to an audience of nurses in May 2005, then Minister of Health George Smitherman explicitly recognized the problems of worker safety in this sector:
One of the things I was struck by…[was] the number of nurses that work in environments, hospital environments most particularly, that actually are unsafe…We have a lot of work to do on that.
We know that even though occupational health and safety legislation has applied to our workplaces since 1979, few health-care employers understand occupational health and safety principles and law, and very few have properly functioning and effective Joint Health and Safety Committees (JHSCs). Our complaints and concerns were resoundingly affirmed by the late Justice Archie Campbell in his final report of the Severe Acute Respiratory Syndrome (SARS) Commission Inquiry. In January 2007, he wrote:
Hospitals are dangerous workplaces, like mines and factories, yet they lack the basic safety culture and workplace safety systems that have become expected and accepted for many years in Ontario mines and factories and in British Columbia’s hospitals.
The 2007 Coroner’s Inquest into the tragic workplace murder of ONA member Lori Dupont also confirmed that health and safety problems continue in our workplaces requiring changes and attention by employers and government.
ONA has been working diligently to change this state of affairs and entrench health and safety cultures in the health-care sector. We have negotiated occupational health and safety language in collective agreements and have independently, and in collaboration with others, pressed the government to improve laws and increase enforcement. We have launched membership initiatives and training. This is to improve JHSC functioning, to combat violence, infectious disease and other hazards in the workplace, and to return our injured and otherwise disabled members to work that is safe for them to do. Activists have been sharing concerns and strategies for addressing all of these issues. As a result, the government and some employers have listened and we now have more lifting devices, needle safety legislation, government-funded and mandated N95 respirators, Workplace Safety and Insurance Board acknowledgement of the need to apply health and safety law and principles to injured workers, plus the precautionary principle has been enacted in legislation (Health Promotion and Protection Act sec. 77.7 (2)).
With ONA pressure, the Ministry of Labour, Training, and Skills Development (MLTSD) (formerly known as the Ministry of Labour MOL) has been more active in our workplaces. The Ministry has issued thousands of orders addressing all forms of hazards in our workplaces and since 2003, has successfully prosecuted several health-care employers for occupational health and safety infractions.
In facilities that have received enforcement attention, we are seeing the beginnings of health and safety cultures and some decrease in injuries. ONA’s health and safety activists are sharing information/experiences and report successes.
There has been progress, but not enough of it. ONA’s health and safety consciousness has risen with more and more of our members identifying hazards and issues. ONA has pursued even more appeals of MLTSD orders/decisions and called for greater enforcement to protect members. We have posted orders and charges and convictions on our website to let members know what can be done, and to publicize these enforcement actions to promote general deterrence of non- compliant employers throughout the sector.
Unfortunately, the introduction of COVID-19 has reinforced how we need to continuously work to ensure proper protections are in place for health-care workers (HCWs). As Justice Archie Campbell said, “Hospitals are dangerous workplaces;” unfortunately, we learned that his recommendations were not implemented and sustained post-SARS. ONA continues to be at the forefront of advocacy for health and safety, filing grievances, filing appeals at the Ontario Labour Relations Board (OLRB), and lobbying the government for better personal protective equipment (PPE) among other actions. ONA will persist in supporting our H&S activists to build a culture of health and safety in their facilities to ensure we continue to protect the health and safety of all workers.
What is the Internal Responsibility System and where did it originate?
In the 1960s and 1970s, workers became increasingly dissatisfied with the state of health and safety in their workplaces. An important event in Canadian occupational health and safety history occurred in 1974 when Elliot Lake miners, alarmed about the high incidence of lung cancer and silicosis among them, engaged in a strike over health and safety conditions. The Ontario government responded by appointing Dr. James Ham to chair a Royal Commission into health and safety in mines. His 1976 report, known as the Ham Commission Report, is considered a seminal work that led the way to the establishment of the Internal Responsibility System (IRS) as the implicit framework around which all modern Canadian occupational health and safety legislation is built.
The IRS that Ham talked about is a health and safety philosophy based on the principle that every individual in the workplace has a role to play in health and safety. Boards of Directors, Chief Executive Officers, managers and supervisors have the greatest responsibilities. In brief, they must first establish safe and healthy workplace policies and systems. They are responsible to ensure that measures, procedures, equipment and training are in place and supported, and must take “every precaution reasonable in the circumstances to protect” workers. Workers then have the duty to work safely and report hazards. A workplace JHSC, comprised of management and worker representatives who are equals, monitors the state of health and safety and makes recommendations for improvement.
Workplace parties are expected to work toward an equal partnership in matters of health and safety, but equal partnership and an IRS does not develop overnight. It has been suggested that as an IRS improves, the level of compliance will move from enforced compliance, through self- compliance to ethical compliance. In ONA’s experience, health-care employers have been slow to fulfill their duties. The “external responsibility system” of enforcement (primarily by MLTSD inspections, orders and prosecutions) can stimulate a sluggish IRS and motivate employers and can be the catalyst for making employers work with workplace parties to establish safe and healthy workplaces.
What makes an IRS successful?
The Ontario government commissioned an independent review of the MLTSD health and safety division in the 1980s. The Mackenzie Laskin study looked at the IRS and found:
For the system to be effective, the complete line of command, from the Board of Directors through the chief executive, managers, supervisors and workers, must be accountable for health and safety in the workplace. Support from the top is vital; the Chief Executive who sets health and safety as an equal and integral part of the management process, along with productivity and cost control, will achieve direct benefits in the form of a better health and safety record, and indirect benefits through improved morale, employee pride in their company and public recognition.
The investigators further commented that a successful IRS needs:
- Commitment by senior management to provide for meaningful worker participation in health and safety
- Access by workers to relevant information on health and safety
- Education and training on health and safety for workers and management
- Consistent enforcement of the Act and meaningful penalties for those who violate the rules.
Some Concerns about the IRS
ONA supports Internal Responsibility Systems that guarantee workers meaningful and equal participation into the decisions which affect their health, safety and well-being. However, as noted above, the IRS does not happen overnight. Most of our workplaces do not have a mature IRS, and the power imbalance within the workplace does not allow for the equal partnership in health and safety that is central and essential to the IRS philosophy.
Until the workplace IRS is at the “ethical compliance” level (and few if any workplaces realistically reach this pinnacle), workers must continue to rely on the “external responsibility system” of enforced compliance with occupational health and safety law.
Unfortunately, many of our employers do not completely understand the top-down nature of health and safety responsibilities (as per Mackenzie Laskin above) and often tell our members that workers are equally responsible for health and safety in the workplace. They are wrong. Employers have ultimate responsibility for ensuring a safe and healthy workplace. Knowing they will be held accountable for not maintaining a safe and healthy workplace will hopefully force employers to fulfill their responsibilities under the Act. It will also provide good reason for them to deal with the worker committee members in good faith and will, therefore, be conducive to the development of a robust IRS. So ONA views the IRS as a supplement to external enforcement, but not as its substitute.
Accelerating the IRS
Many of the health and safety concerns of ONA members have been taking too long to resolve. Unresolved concerns have spent months and even years on JHSC agendas, with no solutions in sight. Given this experience, ONA recommends that, wherever possible, members should use the basic IRS. There is nothing in the law requiring the IRS to grind slowly. Don’t let issues drag on. Members should report health and safety concerns to their supervisor and, if not resolved, to their JHSC member and the union, who should raise the unresolved concern as high as necessary, as quickly as necessary to protect workers. When internal workplace efforts fail, call the MLTSD. For more information, see Appendix H: “Unresolved Health and Safety Concerns: Guidelines re: When to Call the Ministry of Labour.”
How ONA Activists Can Help
Despite our best efforts, much more needs to be done and we need to equip and motivate our on-the-ground activists to keep up the fight. Preventable hazards continue to plague health-care workplaces and injuries from violence, musculoskeletal disorders and falls outpace much of the rest of the workforce, including manufacturing, construction and mining. The health-care sector leads the workforce in illness from reported exposure to workplace contaminants.
Keep in mind that research conducted by the Director of Engineering Services for the Insurance Company of North America suggests a ratio of accident reporting of 1-10-30-600. That means for every reported disabling injury, there are 10 minor injuries, 30 property damage accidents and 600 incidents with no visible injury or damage (“near-miss” accidents). This ratio does not take into account unreported incidents. It can be said that unreported events need the same attention and focus. It is critical for members to report all events, including the “near misses,” to ensure the contributing factors are investigated and appropriate action is taken to prevent an accident from occurring. Using the theoretical ratio above and the reported accident rate, we can begin to extrapolate the real frequency of these occurrences in health care.
Yet the MLTSD seems to pay disproportionate attention to our sector.
ONA participated in the development of a booklet of advice on the types of approaches that can help health and safety activists make the most impact in their workplaces, “Health and Safety Representation, Writing the Workers Back In,” available on ONA’s website (located at https://www.ona.org/wp-content/uploads/loarc_workersguide_201404.pdf). The guidance is based on research and experience of activists and was prepared by occupational health and safety specialists from unions, the Workers Health & Safety Centre (WHSC) and the Occupational Health Clinics for Ontario Workers (OHCOW). Social science research by a core group of these activists revealed, “Ten Operating Principles for Guiding Effective Participation.” (Excerpted as Appendix J in this booklet).
The Law
The Occupational Health and Safety Act
The Occupational Health and Safety Act (the Act) was first passed in 1979 and applies to most workers and workplaces in Ontario. It is designed to protect workers against health and safety hazards in the workplace.
The Act has undergone many amendments since its enactment, but the basic structure and purpose remains unchanged. It sets out general principles and duties for employers, the JHSC, workers and other parties to promote healthy and safe workplaces in Ontario. Individuals, including directors and officers of corporations, face maximum fines of up to $100,000 and imprisonment of up to 12 months, and corporations can be fined up to a maximum of $1,500,000 if found in violation of the Act or its regulations (Section 66).
Regulations
The Occupational Health and Safety Act also gives the Ontario government the power to make regulations, which are more detailed instructions on how the duties of workplace parties are to be carried out. When the first Act was passed in 1979, regulations for industrial establishments, construction projects and mines also came into effect. Since that time, several changes have been made to existing regulations, and additional regulations have been put in force.
In 1993, a regulation for the health-care sector, called the Regulation for Health Care and Residential Facilities, came into effect. Although a draft regulation for the health-care sector was initially completed in 1987 through the efforts of a bipartite committee of labour and management, passage of the regulation had been stalled over government concerns about costs and opposition from the Ontario Hospital Association (OHA). When the provincial government re-opened discussions on the draft regulation in 1991, labour representatives at the table were dismayed to find that many of the provisions of the 1987 draft, which had been determined through a consensus process, were up for discussion again.
Despite the provincial government’s claim of a commitment to occupational health and safety, the end result of this next round of discussions was disappointing. When the new regulation was finally proclaimed early in 1993, important sections were completely left out and other sections were weakened and, therefore, offered less protection. Since then, we have fought to secure legislation to better protect our members, such as needle safety regulations, violence prevention provisions and amendments to the work refusal section of the Act. In September 2016, there were further amendments to the Act expanding employer duties regarding workplace harassment and defining “sexual harassment” as a type of workplace harassment. The violence and harassment provisions still are not perfect, and ONA continues its efforts to ensure there is adequate law to protect our members, and that it is appropriately enforced.
Use the tools and resources in this booklet and the ONA companion booklet Violence in the Workplace, and on the ONA website (www.ona.org) to assist in efforts to enforce these and other parts of the legislation.
Regulation for Health Care and Residential Facilities
This regulation applies to the following types of facilities including, but not limited to:
- A hospital as defined in the Public Hospitals Act or the Community Psychiatric Hospitals Act.
- A laboratory or specimen collection centre as defined in the Laboratory and Specimen Collection Centre Licensing Act.
- A private hospital as defined in the Private Hospitals Act.
- A psychiatric facility as defined in the Mental Health Act.
- A long-term care home as defined in the Long-term Care Homes Act.
- A supported group living residence.
Most other health-care facilities not listed above should be covered under the Industrial Establishments Regulation 851 (see below).
The health-care regulation sets out the employer’s obligation to develop measures and procedures in consultation with the JHSC (Section 8 and 9). The obligation for the employer to develop a written occupational health and safety policy already exists under the Act, but the only regulation in which the measures and procedures to implement the policy are reinforced is the regulation for health care in which there is a list of specific measures and procedures to be addressed. Among other things, the list includes:
- Safe work practices.
- Safe working conditions.
- Proper hygiene practices.
- Control of infections.
- Immunization and inoculation against infectious diseases.
- Biological, chemical and physical hazards.
- The handling, cleaning and disposal of soiled linen, sharps and waste.
The health-care regulation has similarities to the regulation for industrial facilities in that it covers comparable areas, e.g., the requirements for work with scaffolding, and rules about operating machinery, ladders, material lifting equipment, explosives and other hazards associated with work in an industrial setting.
However, O. Reg 420/21, Notices and Reports Under Sections 51 To 53.1 of the Act – Fatalities, Critical Injuries, Occupational Illnesses and Other Incidents states what details an employer must include in reports to the MLTSD concerning workplace injuries and fatalities. These reports are required under Section 51-53 of the OHSA, and the regulation lists mandatory details, such as names and addresses of victims, witnesses, and steps taken to prevent a recurrence.
The health-care regulation also contains detailed rules on hazards specific to health-care facilities, such as:
- Anesthetic gases.
- Antineoplastic drugs.
- Housekeeping and waste.
Section 96 on anesthetic gases outlines the employer’s obligation:
- To install effective scavenging systems to collect, remove and dispose of waste anesthetic gases.
- Install anesthesia machines to reduce contamination of air in the room during administration of anesthetic gases.
- Implement a program to inspect and maintain scavenging systems and anesthesia machines.
- To adopt work practices to reduce contamination of room air with anesthesia
- For the regular maintenance of ventilation systems, including filters.
The regulation does not explicitly require regular air monitoring for anesthetic gas levels, although an earlier draft of the legislation called for monitoring at three-month intervals and whenever requested by workers in those areas.
Section 97 on antineoplastic drugs requires the employer in consultation with the JHSC to develop written measures and procedures to protect workers who may be exposed to antineoplastic agents or material, or equipment contaminated by those agents. Procedures shall include:
Procedures for normal storage, preparation, handling, usage, transportation, and disposal of the drugs and drug-contaminated materials.
- Emergency procedures to be followed if a worker is exposed to the dug.
- Maintenance and disposal of equipment contaminated with antineoplastic agents.
- Measures for the use of engineering controls, work practices and appropriate personal protective equipment
- An appropriate biological safety cabinet for the preparation of antineoplastic drugs.
The section also obliges the employer to provide training and instruction in these measures and procedures to workers who may be exposed to antineoplastic drugs.
Sections 113 and 114 deal specifically with the disposal of sharps and the issue of recapping needles. Section 113 defines “sharps” as “needles, knives, scissors, scalpels, broken glass or other sharp objects” and says these must be discarded in puncture-resistant containers.
Section 114 requires that used needles be discarded immediately after use, without being bent or recapped, into a puncture-resistant container. It does allow for the possibility that there are times when immediate disposal of a used needle into a puncture-proof container may not be practicable. In these cases, the regulation allows for workers to use an employer-provided device to recap needles “that protects workers from being accidentally punctured while they are recapping.” Workers using such devices must be instructed and trained in their use, and although the employer may choose the device, this must be done in consultation with the JHSC or health and safety representative (see also section on “Needle Safety” below).
Regulation for Industrial Establishments
ONA believes this regulation covers virtually all ONA workplaces that are not captured under the facilities identified in Regulation for Health Care and Residential Facilities above. This industrial regulation was one of the original regulations written under the Act, and pre-dated the health care regulation by more than a decade. This regulation applies to a wide variety of workplaces, including factories, shops, offices and arenas, and is heavily oriented to industry. The industrial regulation usually covers health care facilities, such as public health units, community nursing, and blood clinics. While the Regulation for Health Care and Residential Facilities does not automatically apply to such workplaces, it is often argued that the provisions of the health care regulation are “reasonable precautions” to take in any health care workplace, and thus by extension, they too have application to health care workplaces covered by the Regulation for Industrial Establishments.
Needle Safety
A Needle Safety Regulation (O. Reg. 474/07) mandating the use of safety-engineered needles (SENs) or needleless systems to replace hollow-bore needles in hospitals came into effect September 1, 2008. The regulation provides some exceptions to the requirement, and the government has since extended the requirements to long-term care homes, psychiatric facilities, laboratories and specimen collection centres and other health care workplaces, (e.g. home care, doctors’ offices, ambulances, etc.). This legislation applies in addition to the Act and the pertinent provisions of the health care regulation explained above to address health and safety concerns about sharps.
Biological and Chemical Regulations
There are also regulations in place to control toxic substances in the workplace, the presence or use of which may endanger the health or safety of a worker. Regulation 833 – having a hard time finding this controls exposure and sets limits in workplace air for approximately 600 specific biological and chemical agents.
The other approach used by the MLTSD has been to develop a regulation specific to particular toxic substances, such as asbestos, mercury and ethylene oxide. These substances are known as designated substances. Originally, each designated substance had its own regulation, but in 2009 they were consolidated into a single “Designated Substances” regulation 490/09. The regulation contains provisions for an assessment of the likelihood of worker exposure in the workplace and a control program, which includes provisions for engineering controls, work practice, hygiene practices, air monitoring, record keeping and medical surveillance.
Critical Injury – Defined
O.Reg 420/21 – Notices And Reports Under Sections 51 To 53.1 of the Act – Fatalities, Critical Injuries, Occupational Illnesses And Other Incidents defines “critical injury.” There are stricter notice deadlines under Section 51 of the OHSA (immediate verbal notice and 48-hour written notice) for “critical” (and fatal) injuries, than there are for other disabling injuries and illnesses under OHSA Sections 52 (four days) and project or mine events under OHSA Section 53 (two days). Also, a worker member of the JHSC is entitled to investigate “critical” injuries (OHSA Section 9 (31)).
Other Laws
Other pertinent legislative documents members may need to use are:
- Ambulance Act.
- Atomic Energy Control Act.
- Building Code Act.
- Compensation for Victims of Crime Act.
- Criminal Code of Canada.
- Dangerous Goods Transportation Act.
- Environmental Protection Act.
- Fire Protection and Prevention Act and Fire Code.
- Freedom of Information and Protection of Privacy Act.
- Healing Arts Radiation Protection Act.
- Health Protection and Promotion Act.
- Laboratory and Specimen Collection Centre Licensing Act.
- Long-Term Care Homes Act.
- Mental Health Act.
- Occupier’s Liability Act.
- Ontario Human Rights Code.
- Private Hospitals Act.
- Public Hospitals Act.
- Regulated Health Professions Act.
- Transportation of Dangerous Goods Act.
- Workplace Hazardous Materials Information System (WHMIS) Regulation 860.
- Workplace Safety and Insurance Act.
- X-ray Safety Regulation 861.
Workers’ Rights under the Act
The “Three Rights”
In Ontario, Ham’s report led to the enactment in 1978 of the current Occupational Health and Safety Act, which legislated JHSCs and also embodied what has become known as the “three rights” i.e. the workers’ right to know, to participate and to refuse unsafe work. While not explicitly written, these principles are manifested in various sections of the Act.
Right to Know
Workers have a basic right under Section 25 of the Act to know exactly what hazards they are being exposed to at work. Generally, the employer must provide workers and their JHSC or health and safety representative (in workplaces with six to 19 workers) with information and instructions in addressing and improving workplace health and safety. Specifically, all hazardous articles, devices, equipment and biological chemical and physical agents must be identified (Section 37 (1)) and workers must be instructed on how to use, handle and store them safely (Section 37 (3)). For instance, Section 97 of the Health Care Residential Facilities Regulation obligates the employer to provide written instructions to workers with regard to the handling of antineoplastic drugs. Section 9 (4) of the Health Care Residential Facilities Regulation (applicable to hospital and LTCH employers) also requires these employers in consultation with the Joint Health and Safety Committee (JHSC) or Health and Safety Representative to develop, establish and provide training and educational programs in health and safety measures and procedures for workers that are relevant to the worker’s work. Therefore, merely providing information or a few instructions is not sufficient and would not comply with this provision of the regulation.
OHSA Section 32.0.5 (3) states it is the employer’s duty to provide information about violence to a worker under clause 25 (2) (a) and a supervisor’s duty to advise a worker under clause 27 (2) (a). This includes providing personal information related to a risk of workplace violence from a person with a history of violent behaviour if the worker can be expected to encounter that person in the course of their work and if the risk of workplace violence is likely to expose the worker to physical injury.
The Occupational Health and Safety Act and any explanatory material must be posted in the workplace, both in English and the majority language of the workplace (Section 25 (2) (i)). Workers are also entitled to copies of inspectors’ reports and orders (Section 57 (10)), air sampling results, an annual Workplace Safety and Insurance Board (WSIB) summary of deaths, injury and occupational illness in the workplace (Section 12), and any other reports concerning health and safety in that workplace (Section 9, 25 (2) (l) & (m), 51, 52, 53, 59).
Workplace Hazardous Materials Information System (WHMIS)
The “Right to Know” provisions of the Act include language under “Part IV – Toxic Substances,” which establishes the WHMIS. A WHMIS regulation clarifies in detail the provisions in the Act. Since February, 2015 WHMIS across Canada has been undergoing revisions to align it with new international standards for classifying hazardous chemicals and providing information on labels and safety data sheets.
The three major components of WHMIS legislation continue to be:
- Comprehensive labeling of all hazardous materials.
- Provision of Safety Data Sheets (SDS) containing detailed information about the properties of substances, their potential hazards and safe ways of handling such materials.
- Training of workers and supervisors who are exposed or likely to be exposed to hazardous materials or who use these materials in their work.
The main differences are that “controlled products” are now “hazardous products” and as described on the Ontario MLTSD website there are:
- New rules for classifying hazardous workplace chemicals.
- Two main hazard classes – physical hazards and health hazards.
- New label requirements including pictograms instead of symbols that correspond to hazard classes; and
- A different format for safety data sheets.
The key responsibilities of suppliers, employers and workers are the same under WHMIS 2015.
The Globally Harmonized System (GHS) for Hazard Communication is an internationally-accepted standard for the identification of health, physical and environmental hazards in the workplace.
Right to Participate
As explained above, the philosophy underpinning the Occupational Health and Safety Act is known as the “Internal Responsibility System” (IRS). This system assigns authority over occupational health and safety in the workplace to the management, but all workplace parties should be involved in the protection of their health and safety. Workers have responsibilities to work safely. In addition, workers, particularly those selected by the union(s) in the workplace to sit on the JHSC, have an opportunity to shape the health and safety environment in their workplace. The JHSC is the driving force of the IRS in the workplace and the Act confers several powers to facilitate worker participation in workplace health and safety, including, but not limited to:
- Workers select at least half of the JHSC members and a co-chair (Sec. 9 (7) (8)(11)).
- Receive paid time to caucus before meetings, meet and perform JHSC duties (Sec. 9 (34) (35)).
- Write recommendations (Sec. 9 (18)).
- Be present at the beginning of testing (Sec. 9 (18)).
- Inspect the workplace at least once a month (Sec. 9 (26)).
- Investigate fatal and critical injuries (Sec. 9 (31)).
- Accompany an inspector (Sec. 54 (3)).
Without a competent, effective JHSC with the active and sustained participation of workers, the occupational health and safety of the workers in the workplace may be severely compromised.
Right to Refuse or Stop Unsafe Work
The Act provides a conditional “Right to Refuse” unsafe work for health-care workers (Section 43). Health-care workers who work in institutions can refuse unsafe work only when the life, health or safety of another person or the public is not directly in danger.
This conditional Right to Refuse applies to police officers, firefighters, ambulance workers and some other groups of workers who care for the public. The majority of Ontario workers do not have this condition put on their right to protect their own safety in the workplace. Even some health-care workers, such as community health nurses who work outside institutions, have no statutory limitation put on their right to refuse unsafe work. However, there may be consequences related to regulatory body (i.e. CNO) standards.
Certainly no health-care worker wants to jeopardize the life, health or safety of another person, but neither should they be expected by the employer to needlessly jeopardize their own safety. See the ONA guide My Right to Refuse Unsafe Work: A Guide for ONA Members for detailed information about an individual worker’s right to refuse unsafe work. This guide can also be downloaded from ONA website (visit www.ona.org and go to the health and safety section).
The Act also provides a conditional “Right to Stop Dangerous Work” to health-care workers (Section 44-47). Designated JHSC members may initiate a work stoppage, but only in “dangerous circumstances” (Section 44(1)), which means a situation in which all of the following are true:
- The Act or the regulations are being violated.
- The violation poses a danger or a hazard to a worker.
- Delay in controlling the danger or hazard may seriously endanger a worker.
In most cases, it takes two certified members to direct an employer to stop dangerous work. One must be a certified member representing workers, the other a certified member representing the employer. In some special cases, a single certified member may have this right. Sections 45, 46 and 47 of the Act set out the procedure for exercising this right.
The same limitations apply to this right as to the “Right to Refuse” that is, health-care workers and others who work in a variety of health-care facilities cannot initiate a work stoppage if doing so will endanger the life, health or safety of another person (Section 44(2)). This legal condition restricts the rights of health-care workers to stop dangerous work, so if in doubt, members should consult their Bargaining Unit/Labour Relations Officer and their ONA JHSC member or call the MLTSD. (See My Right to Refuse Unsafe Work: A Guide for ONA Members that can be found on the ONA website at www.ona.org)
SARS and the Fourth Right
The rights of workers to know, participate and refuse unsafe work arose from the Ham Commission inquiry into health and safety in mines. Justice Campbell’s SARS Commission findings about health and safety in the health-care sector has suggested a fourth worker’s right: the right to have the “precautionary principle” applied to health and safety in our workplaces.
In the spring of 2003, SARS swept through Ontario, causing 44 deaths and hundreds of cases of lung disease. The province suffered, but the health-care system, particularly in Toronto, was devastated. The government appointed Justice Archie Campbell of the Superior Court of Justice to lead an independent investigation into SARS. Justice Campbell relied heavily on ONA members’ evidence and was open in his praise for the courage of ONA members and other health- care workers who persevered through the crisis. We owe a debt of gratitude to Justice Campbell for his work. His final report, containing more than 80 recommendations, is every bit as important to workplace safety as the work of Dr. Ham in the 1970s.
Justice Campbell’s key recommendation or “take-home message” was the need for adoption of the “precautionary principle, which states that action to reduce risk need not await scientific certainty.” He recommended that it:
be expressly adopted as a guiding principle throughout Ontario’s health, public health and worker safety systems by way of policy statement, by explicit reference in all relevant operational standards and directions, and by way of inclusion, through preamble, statement of principle, or otherwise, in the Occupational Health and Safety Act, the Health Protection and Promotion Act, and all relevant health statutes and regulations.
Calling this, “…the most important lesson of SARS,” he said, “we should not be driven by the scientific dogma of yesterday or even the scientific dogma of today. We should be driven by the precautionary principle that reasonable steps to reduce risk should not await scientific certainty.”
ONA secured an initial victory in 2007 by convincing the government to insert the precautionary principle into the Health Protection and Promotion Act. As a result, now when issuing a directive involving an outbreak, the Chief Medical Officer of Health:
“shall consider the precautionary principle where, b) the proposed directive relates to worker health and safety in the use of any protective clothing, equipment or device” (section 77.7 (2)).
In accordance with the precautionary principle, ONA also convinced the government to mandate the use of and supply N95 respirators in preparation for a pandemic. ONA has also negotiated precautionary principle and N95 respirator language into the Hospital Central and other collective agreements.
This is progress, but not perfection. For the protection of our members and as a tribute to Justice Campbell and his legacy, ONA continues in its efforts to have the precautionary principle widely adopted, and to ensure that the rest of his sage recommendations are implemented.
The Internal Responsibility System within the Occupational Health and Safety Act
The IRS is not overtly mentioned in the Occupational Health and Safety Act, but as discussed above, it is implicit in the Act. The Act gives everyone responsibility for health and safety by assigning specific duties to employers, supervisors, workers and other workplace parties.
In brief:
- Employers are legally required to establish a health and safety policy and program and a safe working environment, ensure every reasonable safety and health precaution is taken to protect workers and ensure supervisors are “competent,” e. familiar with health and safety legislation and have knowledge of potential or actual dangers to health and safety in the workplace.
- Supervisors must ensure the workplace is safe, workers are working safely, every precaution reasonable in the circumstances is taken to protect workers, and any concerns that come to their attention are
- Workers must work safely and report hazards.
- JHSC should address unresolved health and safety concerns and, where appropriate, should:
- CAUCUS with other worker members before every JHSC meeting to discuss concerns, share information and develop written recommendations to present to the committee as a whole (see Appendix D for memo confirming joint union intention for health care unions to work together).
- RECOMMEND actions/solutions in writing to the employer, who has 21 days to respond in writing with a timetable for implementation and reasons for any denial.
- CALL THE MLTSD if a concern cannot be resolved through this IRS (e.g. employer rejects recommendations in whole or part or response is not satisfactory). The MLTSD may issue orders and/or prosecute if there is a violation of the Act or the regulations.
As previously mentioned, don’t let issues drag on. The JHSC should raise unresolved health and safety concerns as high as necessary, as quickly as necessary. When internal workplace efforts fail, call the MLTSD (for more information see Appendix H: “Unresolved Health and Safety Concerns: Guidelines re: When to Call the Ministry of Labour”).
The following sections provide short summaries of parts of the legislation that assign responsibilities and functions to the various participants in the IRS. Please refer to the actual legislation for exact and accurate language.
Duties of the Employer under the Act
(Reference: Section 25 of the Occupational Health and Safety Act)
- Provide information, instruction and supervision to a worker to protect the health or safety of that worker.
- Provide, upon request, information including confidential business information, to a legally qualified medical practitioner in a medical emergency for the purpose of diagnosis or treatment.
- Appoint a competent person to serve as supervisor. “Supervisor” has a specific definition in this At times ONA members, who for instance act as charge nurses or “in-charge or a variety of other positions, either permanent or temporary) may fall within this definition and therefore have the personal legal duties and liabilities of a “supervisor”. “Competent person” has a specific meaning under the Act. A “competent person” is one who must:
- Be qualified through knowledge, training and experience to organize the work and its performance.
- Be familiar with the Act and the regulations that apply to the work being performed in the workplace.
- Know about any actual or potential danger to health and safety in the workplace.
- It is the employer’s duty to ensure that anyone acting in a “supervisor” role in the workplace is trained to meet these legislated requirements to qualify as “competent persons.”
- Acquaint a worker or a person in authority over a worker with any hazard in the work and in the handling, storage, use, disposal and transportation of any article, device, equipment or a biological, chemical or physical agent.
- Offer assistance and cooperation to a committee or a health and safety representative in carrying out their functions.
- Employ in or about a workplace only a person over such an age as may be prescribed.
- Take every precaution reasonable in the circumstances for the protection of a worker.
- Post in the workplace a copy of the Act and any explanatory material prepared by the MLTSD, both in English and the majority language of the workplace, outlining the rights, responsibilities and duties of workers.
- Prepare and (at least) annually review a written occupational health and safety policy and develop/maintain a program to implement that policy, in consultation with the JHSC. Employers are also required to post the policy and provide copies to the JHSC or health and safety representative (Sections 25 (2)(j)(k) of the Act and Sections 8 and 9 of the Regulation for Health Care and Residential Facilities).
- Provide the JHSC or the health and safety representative with the results of any occupational health and safety report the employer has. If the report is in writing, the employer must also provide a copy of the relevant parts of the report.
- Advise workers of the results of such a If the report is in writing, the employer must, on request, make available to workers copies of the portions that concern occupational health and safety.
- Ensure that all equipment required by the Act or regulations is provided, maintained in good condition and used properly by workers.
- Ensure that measures and procedures required by the Act and regulations and employer policy are carried out.
Additional responsibilities of the employer may be found in other sections of the Act:
- Provide a written response to a JHSC or either of the JHSC co-chair’s written recommendations within 21 days. The written response must contain a timetable for implementation and provide reasons for disagreeing with any recommendations (Section 9 (20) (21)). (As a result of a 2011 amendment to the Act, when good faith attempts to reach consensus fail, either co-chair has the power to make written recommendations (Section 9 (19.1) that trigger the duty of the employer to respond in writing within 21 days of receipt of the recommendation.)
- Establish a medical surveillance program for workers as prescribed and provide for safety- related medical exams and tests, and related expenses and wages (Section 26 (1) (h) (i) (3)).
- Prepare policies and programs on workplace violence and harassment, and assess and reassess the risk of violence as often as necessary to ensure the violence policy and program continue to protect workers from workplace (Sections 32.0.1 – 32.0.8)
- Notify the MLTSD, JHSC, health and safety representative and trade unions within 48 hours when a worker is critically injured or killed (Section 51).
- Notify the MLTSD (if required), JHSC, health and safety representative and trade unions within four days when a worker is disabled or requires medical attention resulting from an accident, fire or explosion or incident of workplace violence (Section 52 (1)).
- Notify the MLTSD, JHSC, health and safety representative and trade unions within four days of being advised of an occupational illness (Section 52 (2) (3)).
- Where a notice or report is not required under Section 51 or 52 and an accident, premature or unexpected explosion, fire, flood or inrush of water, failure of any equipment, machine, device, article or thing, cave-in, occurs at a construction project, notify the MLTSD, JHSC, health and safety representative and trade unions in writing within two days of the occurrence (Section 53).
- Afford a worker JHSC member an opportunity to accompany an inspector during a physical inspection of the workplace (Section 54 (3)).
- Provide the JHSC and health and safety representative with copies when the Ministry inspector finds violations of legislation and issues order(s) (Section 57 (10)).
Employer Reprisals
Employers are prohibited by Section 50 of the Act from taking any disciplinary action against an employee or intimidating them because they worked in compliance with the Act, the regulations or an order made under the Act. Employees are also protected by the Act if they are seeking enforcement of the Act or its regulations. If an employer does violate the Act and takes prohibited action against a worker, the worker has the option of filing a grievance under the collective agreement and having the matter dealt with by final and binding arbitration, or by filing a complaint with the Ontario Labour Relations Board.
Duties of the Supervisor under the Act
(Reference: Section 27 of the Occupational Health and Safety Act)
- Advise a worker of the existence of any potential or actual danger to the health or safety of the worker of which the supervisor is aware.
- Take every precaution reasonable in the circumstances for the protection of the worker.
- Ensure that a worker works in the manner and with the protective devices, measures and procedures required by the Act and the regulations.
- Ensure that a worker uses or wears the equipment, protective devices or clothing the employer requires.
- Provide a worker with written instructions regarding measures or procedures to be taken for the protection of the worker, where prescribed.
It is essential that supervisors fully understand their duties under the Act in order to properly address our members’ health and safety concerns. Employers have a responsibility under the Act to ensure that all its supervisors are competent. Nurses, like many other unionized professionals, often end up directing or supervising other workers. ONA therefore expects and requests that all employers provide full training for all supervisors, including ONA members working in a supervisory capacity (as defined in the Act) on matters within their responsibility. This must include ensuring that the workplace has a full set of policies and protocols for handling all potential health and safety situations and concerns, and ensuring that supervisors are fully trained in their application.
The Public Services Health and Safety Association (PSHSA) and the Workers Health and Safety Centre (WHSC) have courses in supervisor competency, as do other providers. Where lacking, the JHSC or either co-chair can make a written recommendation to the employer to provide the needed training to make supervisors “competent” under the Act. For sample recommendations, see Appendix B.
Duties of the Worker under the Act
(Reference: Section 28 of the Occupational Health and Safety Act)
- Work in compliance with the provisions of the Act and the
- Use or wear the equipment, protective devices or clothing the employer
- Report to the employer or supervisor the absence of/or defect in any equipment or protective device of which they are aware and which may endanger themselves or another worker.
- Report to the employer or supervisor any contravention of the Act or the regulations or the existence of any hazard of which they (See Health Safety Hazard Report Form).
- Do not remove or make ineffective any protective device required by the regulations or the employer without providing an adequate temporary protective device, and when the need for removing or making ineffective the protective device has ceased, replace the protective device
- Do not use or operate any equipment, machine, device or thing, or work in a manner that may endanger themselves or any other
Duties of Directors and Officers of a Corporation
(Reference: Section 32 of the Occupational Health and Safety Act)
- Take all reasonable care to ensure that the corporation complies with the legislation and orders and requirements of inspectors, directors and the
Courts expect directors to “immediately and personally react when they have notice that the system has failed” (Making Lemonade out of Lemons, Ontario Federation of Labour, May 2007, page 6). Many corporate leaders aware of these responsibilities have signed on to a national Health and Safety Leadership Charter to provide mutual support and encouragement in meeting workplace health and safety challenges.
A similar awareness is not widespread among board members and executives in Ontario’s health care sector. When the Internal Responsibility System in a workplace breaks down, unions can write to boards of directors explaining the unresolved health and safety concerns in the workplace and pointing out the board members’ personal, individual responsibility to take steps to rectify the situation (for a sample letter, see Appendix C or log onto the members’ section of the ONA website at www.ona.org and follow the links to the health and safety section).
Structure and Functions of the Joint Health and Safety Committee and the Role of the Worker Member
(Reference: Sections 8 and 9 of the Occupational Health and Safety Act)
Structure
- The Act requires workplaces with 20 to 49 employees to have a JHSC (Section 9 (2)) with a minimum of two members on the Where 50 or more workers are employed, the committee must have at least four members. Workplaces with between five and 20 employees are required to select an employee health and safety representative.
- The Minister of Labour may order one JHSC for a multi-site facility (Section 9 (3.1)).
- At workplaces with less than 20 workers, but more than five, a JHSC is not required, but the workers must select at least one non-management health and safety representative from among them (Section 8 (1)). The designated health and safety representative has similar rights and powers as JHSC members (Section 8).
- At least half of the JHSC members shall be workers who do not exercise managerial functions, selected by the union(s) in the
- Management and worker representatives on the JHSC shall each designate one of their members to act as a co-chairperson.
- At least two committee members – one representing the employer and one representing workers – must be chosen for training to become Certified members have specific authority and responsibilities and play a key role on the committee (see the section on “Certification Training,” below). Some unions bargain for greater representation. ONA’s hospital central agreement has a provision requiring certification training for all ONA JHSC members upon written request (article 6.05 (a) (ix)). Members should check their respective collective agreements to see if they are entitled to similar enhancements in their workplaces, and/or negotiate similar provisions.
- JHSC meetings must be held at least every three months, *but often are held
*Meetings may also be convened at the call of either co-chairperson.
- *Guests may be invited to attend a meeting with prior notice and the agreement of both co- chairpersons.
- Worker members will be given time from work to attend all meetings of the All time spent attending JHSC meetings will be considered as work time and members will be paid for this time at their regular or premium rate, as may be appropriate.
- All members of the JHSC should be given paid time off work, as necessary, to carry out their responsibilities between regular committee
- Preparation time, one hour in duration or longer as the committee determines, should be provided as necessary to all members of the JHSC to prepare for a committee Committee members will be paid for this time. Worker members should use this time to caucus with other members from ONA and other unions to discuss issues and prepare written recommendations to table at the main committee meeting.
- The names and work locations of the committee members must be posted in the workplace, where they are most likely to be seen by the The employer is responsible for posting this information.
- Recommendations only; not explicitly mandated by
Functions
- Identify and make recommendations on situations that may be a source of danger or hazard to workers and recommend improvements pertaining to the health and safety of workers in the An employer who receives a written recommendation from the committee, or either co-chair following failure of good faith attempts to reach consensus of the committee, must respond in writing within 21 days. The response must include a timetable for implementing the recommendations. The employer is obliged to provide written reasons for not accepting any recommendations.
- Recommend to the employer, the establishment, maintenance and monitoring of programs, measures and procedures for health and safety in the
- Obtain information from the employer regarding identification of potential or existing hazards and health and safety experience, as well as practices and standards in similar workplaces (Section 9 (18) (d)).
- Obtain information and be consulted about the conducting or taking of tests of any equipment, machine, device, article, thing, material or biological, chemical or physical One of the committee members present at the beginning of testing will be a worker representative (Section9 (18) (f), 11).
- Inspect the workplace at least once a month (worker member designated by JHSC worker members). In many of our workplaces only a portion of the workplace is being inspected monthly versus inspecting the entire workplace. These employers are telling the JHSC worker members that it is not possible to inspect an entire hospital/workplace monthly given its The Occupational Health and Safety Act states “If it is not practical to inspect the workplace at least once a month, the member designated under subsection (23) shall inspect the physical condition of the workplace at least once a year, inspecting at least a part of the workplace in each month.” The question then is, what does “not practical mean”? The MLTSD historically has taken the position that almost all workplaces, including hospitals are not too large to inspect the entire workplace monthly. Therefore, to ensure hazards are being identified and resolved in a timely fashion it is ONA’s position that our ONA JHSC members should be asserting to the employer that it is in fact practical to inspect the entire workplace monthly so long as the employer provides the designated worker member with the time off to do so. If the worker members of the JHSC meet resistance and the employer will not pay for time off to inspect the entire workplace monthly, please contact the MLTSD to file a complaint and advise your Bargaining Unit President and/or LRO that you have done so. Keep in mind, according to the OHSA a worker member of the JHSC will be given time to inspect the workplace. The worker member will be supplied with necessary information and assistance as required for the purpose of carrying out an inspection of the workplace. In multi-site facilities with a single Minister-ordered JHSC, the Minister may permit the worker members of the committee to designate a non-member to conduct inspections (Section 9 (3.2)).
- Participate in designated substance assessments and in the development of control programs under these
- Be consulted by the employer about the development and maintenance of a program regarding workplace harassment (Section 0.6 (1)).
- Request, receive and review Safety Data Sheets (SDS) for hazardous substances used in the
- Be consulted by the employer about making SDSs available in the workplace (Section 38 (6)).
- Be consulted by the employer about the development and implementation and annual review of instruction and training required for a worker exposed or likely to be exposed to a hazardous material or hazardous physical agent (Section 42).
- Review accident and illness reports and statistics and other related information, with a view to preventing future occurrences (Section 12, 51, 52, 53, Occupational Health and Safety Act (OHSA) and Section 3, Notices and Reports Under Sections 51 To 53.1 of the Act – Fatalities, Critical Injuries, Occupational Illnesses And Other Incidents). Many health care employers have not been meeting their reporting obligations and in many cases have only provided the JHSC with summaries of accidents. Many have wrongly claimed they cannot comply because of privacy If your employer refuses to provide you with the information prescribed by Section 3 of the regulation within the time limits set out in Sections 51-53 of the Act, refer them to the MLTSD letter found in Appendix A. If the employer still refuses to provide the required information, call the Ministry of Labour, in consultation with your Bargaining Unit President and Labour Relations Officer.
- Receive and review the results of all inspections and monitor assessment and investigation reports.
- *Ensure the education of workers on safe practices and hazards of the
- *Receive and review new health and safety directives, policies and procedures issued by the government.
- *Review studies and programs regarding occupational health and safety
- Identify issues appropriate for discussion by the
- *Develop a strategy for the provision of information to all levels of
*Recommendations only; not explicitly mandated by legislation.
Worker Member
- The inspecting worker member will inform the JHSC of situations that may be a source of danger or hazard to workers and the committee will consider such information within a reasonable period of
- A worker member(s) of the JHSC will be designated to investigate fatalities and critical injuries. The member(s) chosen to investigate can inspect the actual scene of the accident, but cannot alter it without permission from an They can also inspect any machine, equipment, substance, etc. that may be connected with the accident. They also may question witnesses to the accident, if those persons are willing to be interviewed by the designated worker member.
- A designated worker member will review investigation reports of all fatal and critical injuries and illnesses, and report the findings to the committee who should develop recommendations for future
- *A designated worker member should be given time to assist management in the investigation of all lost time due to workplace injuries and illnesses, and any “near misses,” which are potentially
- A worker member or members of the JHSC will be given time from work to accompany MLTSD officials during inspections and investigations of the
- A worker member will be given time to be present at any investigation into a work refusal and will attend such an investigation without
*Recommendations only; not explicitly mandated by legislation.
Worker Inspections of the Workplace
- The Occupational Health and Safety Act provides the right to designated worker members of the JHSC to inspect the These inspections should be carried out at least once a month.
- In multi-site facilities with a single Minister-ordered JHSC, the worker members of the committee may be advised to designate a non-member to conduct inspections. That designate would have all the powers and rights of a JHSC member (Section 9 (3.2) (3.3)).
Inspection Guidelines
- In some facilities, inspections may be performed by an inspection team consisting of representatives from both management and An arrangement such as this may be set out in the committee’s “Terms of Reference,” which details rules governing the work of the committee. However, the Act requires only that a committee member representing workers perform the inspection (Section 9(23) (26)). And there is no requirement in the OHSA for a committee to have “Terms of Reference.” (For a sample “Terms of Reference,” see Health and Safety section of ONA website at www.ona.org)
- The inspecting worker should identify safety hazards and health hazards present in the workplace and report to a supervisor before leaving the They should review the unit’s accident/injury reports (to which they are entitled) before conducting an inspection as they are a good starting point for determining the most pressing problems in an area. As well, they should be aware of recent staff concerns that have been communicated to them by members working on that unit, such as an increase in violence, back injuries, needlestick injuries, a lack of protocols for the handling and administration of cytotoxic drugs, inadequate ventilation, lack of training, etc.
- For example, when staff concerns such as needlestick injuries are brought to the inspecting worker’s attention, they should record details, including the unit where the needlestick injury occurred, the procedure being performed, patient interference with the procedure, the type of sharps device being used, This information should then be taken back to the JHSC to analyze, with the intention of making a recommendation for the removal of unsafe sharps devices by replacing them with safety-engineered sharps devices.
- A block diagram of the different areas to be inspected will facilitate the identification of a hazard, where it is present and who is exposed or likely to be The block diagram is a floor plan of a work area, such as a nursing unit. It shows location of all equipment, chemicals, drugs, isolation rooms, storage areas, doors, windows and the location of workers.
- Inspection software is available and several large facilities use handy pre-programmed tablets with information including identification of the area, previous inspection reports,
- The inspecting worker should list the substances, physical hazards and processes present or utilized in each work They can ask the workers in the area if they are aware of any hazards to their health and safety or to their co-workers’ health and safety. They should also ask workers if they reported these hazards to their supervisor. If so, what action was taken if any? They may need to work hard to elicit information about hazards and concerns. It has been ONA’s experience that too often health care workers believe that hazards are just part of the job and, as such, may not recognize or report problems that can in fact be reduced or eliminated, and that workers must by law report. The inspection is a perfect opportunity not only to obtain information from workers, but also to educate them about their legal duties to report hazards, faulty equipment, etc.
- The worker can also monitor employer programs and ensure that workers have received appropriate Where training was provided, check that workers have retained their knowledge/skills (e.g., workers who have been fit tested for a respirator should be able to confidently confirm that they remember how to put it on and take it off, indicate which respirator they were fitted for and when one should be used).
- The WHMIS program ensures that products are adequately labeled, providing information regarding their The employer must supply this information by providing Safety Data Sheets (SDS). The SDS, which is obtained from the supplier or manufacturer of the product, provides advice on the short-term or acute effects of exposure to the product but may not provide information about long-term or chronic effects. It is important for the inspecting worker to know that additional information may be obtained from sources, such as the Canadian Centre for Occupational Health and Safety (CCOHS), the WHSC, the PSHSA and ONA.
- The inspecting worker should review protocol or procedure book recommendations, if any, to determine whether current procedures adequately protect workers carrying out a process or procedure (e.g., appropriate infection control measures).
- More and more of our members require accommodation of their disabilities in the Return to Work or modified work plans are negotiated by workplace parties. During workplace inspections, the inspecting worker should review the work of accommodated members to ensure they are working safely within their restrictions and that proper equipment, and all accommodation arrangements are available.
- Also, during the inspection, or at any other time when an accommodated worker raises a health and safety concern, the JHSC and Bargaining Unit representative should work to ensure the worker’s ongoing In some cases, an injured or ill worker may stop working because of pain from the work or because they believe the work will further harm them. Union leaders and JHSC members should be alert to such situations, which may actually constitute work refusals under the Act (for more information about handling concerns of our working injured and ill members, see Appendix F, Safe Return to Work Algorithm, and ONA booklet, My Right To Refuse Unsafe Work: A Guide for ONA Members).
- In our experience, when accommodating workers, employers rarely consider applying a lift program, which includes training and the purchase of ergonomic equipment, and more often than not, they simply attempt to accommodate workers with graduated hours or a buddy system. This may be suitable for some truly temporary accommodations, but in permanent arrangements, ergonomic equipment must be If the worker is having difficulties, an inspecting worker can report this to the committee, which may identify the lack of a safe lift program, training and equipment, such as mechanical lifts and ergonomic supplies that could adequately accommodate the worker (consider revising the sample Lifting Recommendation at Appendix B).
- Following any inspection/investigation, the inspecting worker should report identified hazards to a supervisor and then meet with other worker members of the JHSC to review the inspection/investigation Health and safety hazards noted in the inspection should be discussed, possible solutions to unresolved issues developed and written recommendations drafted (for sample recommendations, see Appendix B). The inspecting worker should then take the report and recommendations to the next full committee meeting, and the full committee should consider possible solutions and make written recommendations to the employer. Following failure of good faith attempts to reach consensus, the worker co-chair can submit written recommendations to the employer independently, to which the employer is obligated to reply in writing within 21 days.
Role of ONA Health and Safety Member on the JHSC
The health and safety member on the JHSC:
- Is elected/selected by the
- Has a working knowledge of the Occupational Health and Safety Act, regulations and available If the JHSC member feels they need more information and/or resource materials, they should contact their Bargaining Unit President and/or LRO for support.
- Responds to the health and safety concerns of members and all workers seeking
- Attends all JHSC meetings and worker caucus preparation
- Takes unresolved health and safety concerns to the JHSC for resolution and advocates for recommendations in writing that will resolve A sample recommendation can be found in Appendix B, or for more sample recommendations, log onto the members’ section of the ONA website at www.ona.org and follow the links to the health and safety section.
- Reports back and maintains close contact with the Bargaining Unit Leadership team regarding health and safety
- May act as co-chairperson of the
- Ensures that JHSC meeting agenda items are submitted in time for discussion at the
- Participates in workplace inspections, as required, and identifies hazards to supervisors and the committee to engage it in finding solutions to eliminate those
- May participate in the development and distribution of JHSC’s meeting
- May record and distribute JHSC meeting
- Liaises with the Bargaining Unit’s negotiating committee regarding improvements to the collective agreement in the areas of occupational health and safety and workers’ compensation.
- Liaises with the health and safety representatives of other local unions in the
- Caucuses with other health and safety committee members from other unions before meetings to gain consensus on approaches to
- May contact the MLTSD if the IRS fails and health and safety concerns remain
- Has completed at least a basic occupational health and safety course (strongly recommended).
- Assists in carrying out the mandate of the
- Acts as the certified worker when selected by worker members of the
- May network with other JHSC members in other ONA
Administrative Process of the JHSC
- The JHSC should develop “Terms of Reference” (a template can be found on the ONA website at ona.org under health and safety) that augments the Act and sets out rules governing the work of the committee. Terms of Reference are not required by the Act, but are a good idea, need to be mutually agreed to with the employer, and should be reviewed annually. Be cautious of developing Terms of Reference that end up delaying the resolution of health and safety concerns through quorum issues.
- The committee should reinforce the cooperative solving of health and safety problems and facilitate information dissemination among workers and
- Any worker may raise a concern verbally or in writing regarding health and safety in the workplace. If possible, health and safety issues should be addressed to the worker’s immediate supervisor before they are brought to the
- Unresolved health and safety concerns should be brought to the JHSC for discussion and resolution. Unresolved concerns should be raised as high as necessary as quickly as necessary to protect
- In the Terms of Reference, the committee can establish the quorum necessary to conduct business and indicate that all issues should be resolved by consensus, not by
- The chairpersons should agree on an agenda and forward a copy to all committee members at least five working days prior to the A provision should be made to allow additions to the agenda with shorter notice or additional emergency meetings where pressing circumstances exist. This procedure should be set out in any Terms of Reference.
- One JHSC member should be designated to record minutes of proceedings at all committee meetings. In some facilities, the employer may provide a secretary to perform this
- ONA JHSC members should ensure that all problems, resolutions, timeframes and responsibility for action are accurately recorded in the
- In the event of disagreement over an individual agenda item, the differing positions should be recorded in the
- Minutes should be signed by both co-chairs or their alternates, who are responsible for ensuring the signed minutes are posted, circulated to all committee members and senior management, and filed at the
- Minutes should be
- All recommendations of the JHSC or either co-chair should be forwarded in writing to the employer for a response in writing within 21 days (Section 9 (20)). Usually this is the CEO or Health Administrator and should not be confused with the employer members sitting on the JHSC, the occupational health and safety department, or
- Efforts should be made to promote cooperation among representatives from all unions representing workers on the (See Appendix D for a joint union memo affirming health- care union commitment to work together in health and safety.)
Role of the MLTSD in Occupational Health and Safety at the Workplace
The Occupational Health and Safety Act is administered by the MLTSD’s Occupational Health and Safety branch, and health care facilities are usually inspected by regional safety inspectors who may be aided by health care inspectors from the branch’s Health Care Unit. See contact information at Appendix G Resources.
Inspector’s Powers
Under Section 54, an inspector has the authority to:
- Enter any workplace without a warrant or
- Question any person, either privately or in the presence of someone else, who may be connected to an inspection, examination or
- Handle, use or test any equipment, machinery, material or agent in the workplace and take away
- Examine documents or records and remove them from the workplace to make copies; this also includes the taking of
- Require that any part of a workplace or the entire workplace not be disturbed for a reasonable period of time to conduct an examination, inspection or
- Require that any equipment, machinery or process be operated or set in motion or that a system or procedure be carried out that may be relevant to an examination, inquiry or
- Examine and copy material concerning workers’ training
- Direct a JHSC member representing workers, or a health and safety representative, to inspect the workplace at specified
- Seize articles permitted by a
- Require the employer, at its expense, to have an expert test and provide a report on equipment, machinery, materials, agents, etc. This also includes having a professional engineer test equipment or machinery and verify it is not likely to endanger a worker or to stop use pending such test
- Require an employer to provide information about any process or agent used in the workplace, or intended to be used there, and the manner of its use, which includes information on ingredients, composition and properties of the agent, toxicological effects of the agent, effects when exposed to skin, inhaled or ingested, and the protective and emergency measures that would be used in the event of
In addition, an inspector may order an employer to conduct, at the employer’s expense, an investigation of a complaint of workplace harassment (Sections 32.0.7, 55.3).
An employer must afford a worker member of the JHSC, selected by the workers, an opportunity to accompany an inspector on an inspection (Section 54 (3)). In smaller workplaces, the health and safety representative must be given the opportunity. If neither is available, the union(s) must be given an opportunity to select someone, and where there is no union, workers must be permitted to select someone. The worker must be considered at work during the inspection and paid at the applicable rate of pay.
In the event that no such worker is available for the inspection, the inspector must endeavor to consult with a reasonable number of workers about their health and safety concerns.
An inspector can also be called in to investigate a complaint. Remember, given that our members’ right to refuse unsafe work is likely limited, the only thing standing between them and imminent jeopardy may be a call to the MLTSD. Because our members have a limited right to refuse unsafe work, the MLTSD has committed to responding to our members’ complaints on a “priority complaint basis” (see confirming memo at Appendix E).
Inspector’s Orders
Where violations have occurred, the inspector may issue written orders to the employer to comply with the law within a certain period of time or, if the hazard is imminent, to comply immediately. An inspector’s order may require the employer to submit a plan to the Ministry, specifying when it will be complying with the order (Section 57).
An inspector may direct a designated JHSC worker member to inspect all or parts of the workplace at specified intervals (Section 55).
An order may also be issued to an employer – with five or fewer workers – to write and post workplace violence and harassment policies (Section 55.1).
In addition, an inspector may order an employer to engage, at the employer’s expense, a third- party to investigate a claim of sexual harassment (Section 55.3).
When an order has been made to correct a violation of the Act or regulations and the violation in question is dangerous to the health or safety of a worker, the inspector may also order the following:
- Any place, equipment or machinery, material process, not be used until the violation has been corrected.
- The work be
- The workplace be cleared of workers, and access to the workplace be prevented until the hazard is
- Any hazardous chemical, physical or biological agent not be
Compliance with a “stop work” order is only established by the inspector personally, which may result if a committee member representing workers advises the inspector that compliance has been achieved.
Within three days of compliance with a regular order, the employer must submit a notice of compliance to the MLTSD, including a statement by a worker JHSC member agreeing, disagreeing or a statement from the employer indicating the worker member declined to sign. Compliance ultimately is decided by the inspector. (Section 59)
The employer is also required to post both the order and the notice of compliance for 14 days in a location where they are most likely to be seen by the workers.
Appeal/Prosecution
An inspector’s order, or decision not to issue an order, can be appealed by a worker, union, employer, constructor, licensee or owner aggrieved by the order. According to Section 61 of the Act, an appeal can be made to the Ontario Labour Relations Board (OLRB) in writing within 30 days after making the order/decision.
The OLRB will assign a Labour Relations Officer to attempt mediation, and if that fails, will send a “Notice of Consultation or Hearing” to all parties. Once an application to appeal has been filed, a party may also apply for a suspension of the order pending disposition of the appeal. The Act gives “all the powers of the inspector” to the Board, and the Board may substitute its findings for that of the inspector, may affirm or rescind an order and substitute a new order (Section 61).
In some circumstances, the MLTSD may also initiate a prosecution, charging the employer and/or supervisor and/or any other party with a violation of the legislation. If the government refuses to prosecute an employer for violating the legislation, an individual or a union can file charges before a Justice of the Peace if there is sufficient evidence to establish reasonable and probable grounds to believe an offence has been committed.
Hazardous Conditions and Substances
Nurses and other health-care workers are often exposed to both safety and health hazards at work. Some hazards are actual, others potential. Some have acute effects, some chronic and some both. The following describes some of the safety and health hazards that affect nurses.
Safety Hazards
A safety hazard is something that has the potential to cause an injury. Occupational injuries are usually the result of accidents. Accidents usually occur when a hazard is not adequately controlled.
Poorly maintained equipment, unsuitable equipment, insufficient staffing, poorly designed work areas, inclement weather, violent patients/residents/clients and poor channels of communication all can contribute to a working environment full of safety hazards to nurses.
Many nurses and other members are injured. They hurt their backs and sustain other musculoskeletal injuries while lifting and moving patients/residents/clients. They are especially at risk of being exposed to diseases such as Hepatitis B, C and HIV from needlestick and sharps injuries. They are involved in motor vehicle accidents while travelling between clinics/clients. They are assaulted by patients/residents/clients and visitors (either verbally or physically, and either may constitute violence in the workplace). They are injured while working alone because there is no one to help them or because they did not know they needed help.
Historically, employers and even other workers have placed the blame for accidents on “careless workers.” A number of Canadian, British and American studies have disproved this widespread belief in what has become known as “behavior based safety – BBS.” Unfortunately, few employers have paid attention to these studies, although researchers have demonstrated that if you dig deeper to the root cause of an accident, you will usually find social or physical conditions in the workplace that led to the accident.
The WHSC has produced an excellent video entitled, Hazards of Behaviour Based Safety, which can be viewed on YouTube at: https://www.youtube.com/watch?v=kdXvnCDbmfg.
Workplace inspection and accident investigation and analysis, followed by strong corrective action and enforcement, are key to the reduction and elimination of safety hazards at work. It has also been demonstrated that training employees to perform a procedure safely and modifying the work environment and equipment does prevent accidents. Also, when an injured worker is returning to work, the workplace should be examined as to why injury occurred and if modifications need to be made to prevent re-injury or injury to other co-workers.
Health Hazards
A potential health hazard exists when a worker is exposed to any agent that can cause illness or disease. Occupational illnesses and diseases are those illnesses caused by exposure to a hazard in the workplace. Health hazards may be categorized as physical, chemical, biological, work design or stress hazards. Reproductive hazards also exist in the workplace, which may be caused by physical, chemical or other agents:
- Physical: Physical hazards include plant/building/equipment problems such as tripping and structural hazards, and forms of energy which may harm the body when exposure takes place. Noise, vibration, temperature and radiation are examples of physical hazards that nurses may encounter in the
- Chemical: Chemical hazards occur in a variety of forms (solids, liquids, vapours, gases, dusts, fumes or mists). Examples of chemical hazards frequently encountered by nurses are antineoplastic drugs, anesthetic gases, pharmaceuticals and cleaning and sterilizing chemicals, such as ethylene oxide and
- Biological: Biological agents are living things or substances which can cause illness or disease in They include bacteria, viruses, fungi and parasites. In their daily work, nurses encounter a wide variety of potentially hazardous biological agents, such as hepatitis, tuberculosis, meningitis, influenza and coronavirus.
- Work Design: The design and organization of work can cause harm to a worker by placing stresses and strains on the musculoskeletal The elements of work design include design of workstations, equipment, physical environment and the actual organization of work (known as “ergonomics”). When these elements are not designed to fit those who do the work, the result may be damage to workers’ muscles, tendons, ligaments, nerves and/or blood vessels. These injuries arise mainly from the nature of nursing work. Many nurses work short-staffed, lifting, moving and transferring patients/ residents/clients repeatedly through each shift with little assistance, either from mechanical lifts or other staff.Patient rooms are often small and poorly designed with little room to maneuver, and patients/residents/clients may be combative or uncooperative. Prolonged night shift work has been linked to serious physical conditions such as heart disease and cancer.
- Stress: Workplace stress and burnout are increasing and often result from exposure to a variety of psychosocial hazards in the Working understaffed, working alone in the community, working shifts and functioning in a work environment with a lot of responsibility and little authority, support, or recognition are examples of psychosocial hazards. The health effects resulting from these hazards include migraine headaches, ulcers and other gastrointestinal disorders, and emotional mental health deterioration.
- Reproductive Hazards: A reproductive health hazard is any agent that has a harmful effect on the adult male or female reproductive system or the developing The agent may be a chemical exposure (waste anesthetic gases), a physical exposure (radiation), a biological exposure (German measles) or a psycho-social hazard due to a work practice, such as shift work or inadequate staffing. Hazards manifest themselves in the adult reproductive system through loss of sexual desire, infertility, impotence, mutation in the germ cell (ovum or sperm) and/or miscarriage. When substance causes damage directly to the fetus, it is called a teratogen. Most teratogens reach the fetus by crossing the placental barrier, interfering with fetal growth and development. If the influence is severe, the pregnancy may end in miscarriage. If the fetus survives, it may have a low birth weight, birth defects, or developmental, behavioral or health effects that may not become apparent until a few years after birth.
Routes of Entry of Physical, Chemical and Biological Hazards
- Inhalation: Inhalation through the respiratory system is a prevalent route of entry for workplace hazards, g., cytotoxic drugs, glutaraldehyde, ethylene oxide.
- Ingestion: Ingestion can occur either by swallowing contaminated material or eating with contaminated hands, e.g., salmonella.
- Absorption: Absorption can occur through the skin, a cut or a puncture, or injection g., Hepatitis B, C, HIV and solvents.
Once a health hazard gains entry to the body, it can do damage at three important sites:
- The site of entry (lungs, stomach, intestines or skin).
- The blood or lymphatic system.
- The organs that work at removing the substance from the body (liver or kidneys).
Damage can also be done to other organs, as well as to the bones and the nervous system.
Health hazards have acute and/or chronic effects. Acute effects occur in the short-term after exposure and generally require high levels of exposure. They can be fatal but are often treatable. Chronic diseases often become apparent only after a great deal of damage has been done. The time period between the first exposure to the health hazard and the onset of the resulting disease is called the latency period. The latency period can be as long as 15 to 40 years after the workplace exposure.
Workers should immediately report all exposures and details of the exposure regardless of whether there is immediate injury/illness. The exposure should be reported to the employer, the worker’s doctor, and in writing to the WSIB. If tests show seroconversion or other damage in the future, the member will at least have a record of the occupational exposure that likely caused their illness. As a result, they may be entitled to WSIB benefits.
Principles of Controlling Health Hazards
Once a health hazard is identified and measured, it must be eliminated or reduced through a control program. Controls can be applied in the following three ways, listed in priority order. (This approach is sometimes referred to as the “hierarchy of controls.” These controls are not mutually exclusive, and are meant to work in combination, providing “fail-safes” when one does not eliminate the hazard. This point is particularly important to remember in the health care sector where some managers have revealed their ignorance of occupational health and safety principles and law by suggesting that they can “cherry pick” from the types of controls, e.g., suggesting respirators are sufficient even though simple engineering controls can eliminate or control the contaminant at the source.)
1. At the Source
- Substitution with a less hazardous substance
- Engineering controls (installing, fixing, replacing or redesigning faulty equipment, local ventilation).
- A redesign of the process, practice or procedure.
2. Along the Path
- Housekeeping
- Administrative controls, such as isolation or cohorting of infectious patients and safety procedures, a proper maintenance program.
3. At the Worker
- Barriers, such as personal protective equipment. Education for workers on reasons why needed
- Alarms, such as panic buttons.
Monitoring the Workplace
Monitoring is a method used to measure the quantity of a hazard to which a worker is exposed in the workplace. One example is monitoring an operating room and a recovery room to measure the amount of anesthetic gases present in the air. If nitrous oxide exceeded the permissible exposure as stated in the Control of Exposure to Chemical and Biological Agents Regulation of 25 parts per million over the period of an eight-hour work day, the employer would be in violation of the regulation and legally required to take measures to eliminate excess gas from the work atmosphere. Also doing air quality testing of some building areas may reveal the possible existence of and concentration of mold where members have complained of headaches, dizziness, aggravation of asthma, etc.
Workers have the right to know the hazards they are exposed to at the workplace. Where a worker suspects or knows of a hazard, such as an exposure to a chemical agent that is not being monitored for effective control measures (i.e., air sampling to establish if the gas is leaking), they should report it to their supervisor and can copy their JHSC and ONA Bargaining Unit President. The JHSC should be informed if the supervisor does not follow up and no action is taken. A recommendation can be brought forward by the JHSC and if necessary, the MLTSD may need to be contacted if the employer does not take action to control the hazard. ONA members should press the JHSC for regular monitoring in certain areas, such as the operating room and recovery room, and where ethylene oxide sterilizers are used.
Occupational Health and Safety Education and Training
Certification Training
Under Section 9(12) of the Act, the employer “shall ensure that at least one member of the committee representing the constructor or the employer, and at least one member representing workers, are certified members.”
To be certified, a JHSC member must have completed part two of “Workplace-specific Hazard” training. This training is in addition to part one, “Basic Certification” training. The employer is responsible for ensuring completion of this training, and certification training must be paid for by the employer and conducted by a recognized Safe Workplace Association. Section 9(14) clearly states it is the right of the workers to choose who will be certified.
The MLTSD enforces the Occupational Health and Safety Act requirements for certified members of JHSCs. When a contravention is found, the inspector should issue an order to the employer or constructor to comply with the requirement.
Although the Act requires that only one worker and one manager per JHSC receive certification training, some employers have agreed to train more, and enhanced training rights have been negotiated into collective agreements e.g., Hospital Central Agreement article 6.05 (e) (ix). Many ONA workplaces are 24-hour, 365 day-per-year operations and contain a variety of potential hazards. The employer may agree to train more JHSC members to attempt to have at least one certified committee member in the facility at all times. (It is common in other workforce sectors to find full-time, trained, paid worker health and safety representatives as a result of collective agreement negotiations.)
Some JHSCs have encountered difficulties with the labour members of the committee when the employer agrees to certify only one worker member. Worker members of the committee, who may represent a number of unions as well as unorganized workers, have had difficulty resolving who will receive training. Strife of this kind is unfortunate, often disrupts the regular work of the committee and may provide the employer with an excuse to resist complying with other health and safety obligations. As much as possible, labour members of the JHSC should work together to develop a strategy and long-term plan around certification training. As well, ONA members with enhanced training rights in their collective agreements, e.g., hospital members, should seek enforcement of those provisions.
If ONA JHSC members have questions and/or concerns about certification training, they should contact their Bargaining Unit President/Labour Relations Officer.
Other Training
The WHSC and the PSHSA are two “Safe Workplace Associations” funded by WSIB and both have numerous training programs that can benefit health care sector workers. Lifting and ergonomics, JHSC functioning, supervisor competency, anesthetic gases, violence prevention, behavior-based safety and radiation safety are just some of the subjects covered in courses offered by these organizations.
For more information about programs and training available from the WHSC and PSHSA, contact the organizations at the numbers or e-mail addresses provided at the back of this guide.
However, the majority of workers who want education in health and safety matters turn to their union first. ONA regularly offers our members workshops on occupational health and safety to assist with basic concepts and prepare a health and safety representative to perform more effectively.
For more information, consult with your Bargaining Unit President/Labour Relations Officer. ONA has historically conducted one-day health and safety caucuses in May of each year in each region. Ask your Local Coordinator/Bargaining Unit President about these.
Make it work for you
How to Use Your IRS
If the IRS in your workplace is working properly, employers, supervisors and workers have fulfilled their responsibilities under the Occupational Health and Safety Act as outlined below:
- The employer has established a sound and comprehensive health and safety policy and program in conjunction with the JHSC, provides health and safety training, information and facilitates the functionality of the JHSC.
- The supervisors are competent by definition under the OHSA. This means they are familiar with the Act and regulations and the employer’s health and safety policies and programs, have knowledge of and advise workers of hazards in the workplace, promptly address members’ health and safety concerns, rectify problems, eliminate and control hazards.
- The JHSC is active, knowledgeable, and consulted on the development and revision of all health and safety measures, procedures and training. The JHSC gathers information, conducts inspections, reviews all accident reports, near misses and statistics to identify hazards and the locations of the The JHSC discusses and investigates issues with a view to making written recommendations to the employer to resolve health and safety issues and to improve the health and safety measures, procedures and training in the workplace. Worker members caucus before each JHSC meeting
- Members are trained about the hazards in the workplace, including the hazardous materials in their areas, and how to protect themselves and When a member has a concern, they raise it with the supervisor, who, as a “competent person” under the Act, resolves the issue. When the matter is not resolved by the supervisor, the member raises it with the JHSC member who caucuses with worker members, discussing solutions and drafting recommendations. The worker members bring it to the attention of the entire JHSC. The JHSC will then make written recommendations to the employer or, after good faith attempts to reach consensus of the committee, either JHSC co-chair will make written recommendations. If the IRS does not resolve the issue, the MLTSD is called upon to resolve disputes and issue orders.
The Ministry inspector will ordinarily ask if the member has exhausted the IRS before they will come to the workplace to investigate the concern. So, if time and circumstances permit, the member should work through the IRS first. But particularly if the issue is longstanding, or danger is imminent, workers should speed up the IRS and elevate unresolved concerns as high as necessary as quickly as necessary and not hesitate to call the MLTSD with a complaint. The member also reports the breakdown of their IRS to the Bargaining Unit/Labour Relations Officer.
See the following diagram on “Internal Responsibility System Procedure for Resolving Health and Safety Problems.”
Examples of the Internal Responsibility System in Action
Sample Scenario 1
A member commences work in a psychiatric unit in a general hospital. A forensic patient with a violent history has been in the unit for the past week, with security attending the patient 24/7. The first day of the admission the patient acted out and with the help of security was restrained and treated. There have been no further actual incidents, but the patient has shown continuing signs of instability. At the beginning of the shift the member is advised that because the patient has stabilized, the security detail has completed their last shift, with no replacement. This unit is chronically under-staffed. This shift, one nurse has called in sick, with no replacement. The unit is therefore short staffed, as well as without benefit of security assistance. Workers on the unit are very concerned about their safety.
What Does the Member Do?
The ONA member reports their concerns to the supervisor, pointing out that it is hazardous to work in this situation without additional staff to aid in an emergency (Section 28 (1) (d)) especially with a known violent patient.
What Does the Supervisor Do?
The supervisor acknowledges the potential danger and advises workers on the unit of the hazard to workers in the area (Section 27 (2) (a) (c), 32.0.5 (3)). They suggest that everyone be careful in approaching this patient, but note that they have been stable for several days and the expense of extra security is not justified. The supervisor reminds them that the patient is the primary concern and they should not have any trouble if they are just sensitive in their handling of them. The response to this concern leaves the member feeling unjustly chastised for poor nursing care and does not address the safety concern.
What Does the Member Do?
The member forthwith raises the unresolved health and safety concern with the ONA member on the JHSC and the Bargaining Unit President.
What Do the ONA Member on the JHSC and the Bargaining Unit President Do?
They begin to raise the concern as high as necessary as quickly as necessary. The Bargaining Unit President calls the unit supervisor’s supervisor who also does not resolve the issue. The Bargaining Unit President continues to climb the chain of command, stating their intent to call the CEO and/or Board of Directors about this imminent hazard if it is not resolved forthwith. When the Clinical Director hears this, they decide to reinstate the security detail overnight, and suggests that the JHSC meet, consider the situation and make recommendations. In this reprieve, the ONA JHSC member raises the issue with the worker co-chair of the JHSC and suggests an emergency meeting of the JHSC.
What Does the JHSC Do?
The union co-chair approaches the management co-chair to call a meeting of the JHSC. The management co-chair refuses to call the meeting, saying the quarterly meeting was held just two weeks ago. The management co-chair cites Section 9 (33) of the Act and the protocol developed by the committee, as authority to deny meetings more than once every three months (Section 9 (18) (b) (c)). The union co-chair expresses their intention to raise this unresolved urgent issue as high as necessary in the employer hierarchy, the union and the government as quickly as required to protect workers from harm. The management co-chair is unmoved, and it appears that the patient is remaining and the unit supervisor has said once again that the security contract has expired.
Now What?
The clinical director acted appropriately in re-establishing security to protect workers in these circumstances, so elevating the unresolved concern as high as necessary and as quickly as required within the IRS worked, temporarily.
But the employer co-chair, in denying a meeting of the JHSC, is wrong. Section 9(33) of the Act requires the committee to meet “at least once every three months,” establishing a minimum, not a maximum, frequency. The employer, who is required by law to take every precaution reasonable in the circumstances for the protection of a worker, still has an opportunity to prevent injuries by using the JHSC. It would certainly be reasonable in this circumstance to meet and fully discuss the hazard and the options.
Regardless of whether the JHSC meets and/or makes recommendations, the employer has the primary responsibility to take every precaution reasonable in the circumstances to protect a worker. With only a temporary “fix,” the IRS did not entirely resolve this issue. Especially given the potential danger of this situation the ONA JHSC member and/or Bargaining Unit President should immediately call the MLTSD to complain of an unresolved safety concern. In this case, it would be wise for the union to impress on the inspector that these workers have a limited right to refuse unsafe work in the workplace. The Union can remind the inspector that because of this limited right, the MLTSD committed to providing a heightened response to health and safety complaints from such workers (for a copy of the MLTSD memo, see Appendix E, or refer to the ONA website at www.ona.org), and that the inspector and their response may be the only thing standing between the member and a serious injury.
The inspector should investigate the complaint and may issue orders.
To assist the inspector, it will help if the member/JHSC member/Bargaining Unit President can cite evidence of infractions (e.g., “My employer does not have a violence program that includes safe staffing measures and procedures, we have no panic buttons. Security was needed to restrain this patient on the first day of admission, nurses x, y and z reported continuing signs of instability, etc.”) If the inspector does not investigate or simply says there is no violation, the member should consult the Bargaining Unit/Labour Relations Officer, who will consider response options including grievances and an appeal of the Ministry’s decision to the Ontario Labour Relations Board (OLRB).
Also, 2010 amendments to the Act clarified that violence and threats of violence by a person are real health and safety issues covered by the legislation. The amendments added the express articulation of the right to refuse work if a worker believes they are at risk of physical injury from “workplace violence,” as it is now defined in the Act. If a worker refuses to work when threatened by such violence, MLTSD will be expected to respond in accordance with the Act. However, because of your regulatory body, you must do so carefully.
Sample Scenario 2
Yet another colleague in a long-term care facility has sustained a serious shoulder injury in the unit; another colleague almost hurt herself themself last night. A member is worried that they will be next.
What Does the Member Do?
The member reports the incident(s) to their supervisor and points out the equipment (bed crank) currently in use may again endanger them or another worker (Section 28 (1) (c)).
The member knows that others have repeatedly reported to the supervisor and their manager that the aging beds with their mechanical cranks are a safety hazard.
What Does the Supervisor Do?
The supervisor shrugs their shoulders and says, “It’s not my problem. That’s why you have a safety committee.” The member is frustrated.
What Does the Member Do?
The member raises the unresolved health and safety concern with the ONA member on the JHSC.
What Does the ONA Member on the JHSC Do?
The ONA member ensures the unresolved health and safety concern is added to the next JHSC meeting agenda, scheduled for the next day, and that sufficient time is allotted to discuss the issue.
CAUCUS: The ONA member encourages all worker members of the JHSC to meet at least an hour before the JHSC meeting to discuss the issue and prepare a joint draft written recommendation. This caucus time is paid time (Section 9 (34) (35)).
The ONA member raises the issue at the JHSC meeting, providing all available information. The ONA member points out that this concern has been raised on numerous units, and supervisors consistently respond that it is not their problem and divert the issue to the JHSC.
What Does the JHSC Do?
The committee asks the employer to provide information about work practices and standards and equipment available and/or in use in other health care facilities (Section 9 (18) (d) (ii)).
After investigating and considering all available information, including accident reports and training records, the committee concludes:
- The old beds are a danger to workers.
- Supervisors in the facility are not “competent” under the Act.
RECOMMEND: The committee makes written recommendations to the employer, which point out that injury reports are high and many are linked to the aging beds. The committee recommends the beds be replaced with electric adjustable beds.
In its recommendations, the committee further points out that the employer is required to ensure supervisors are “competent,” meaning they must not only know how to arrange and direct the work, they must be familiar with the Act and regulations, and the hazards of the work.
The committee highly recommends the employer immediately replaces the beds and institutes a health and safety training program for supervisors in the facility (Section 9 (18) (b) (c), 25 (1) (c) Act, and Section 9 (4), Health Care and Residential Facilities Regulation).
What Does the Employer Do?
The employer immediately sees the error of its ways and responds in writing to the committee’s recommendations the next day, well within the 21 days required by the Act. The employer gives a three-month timetable for the purchase of new beds (and interim measures to prevent injury such as tagging out problem beds where possible) and completion of supervisor safety training.
The employer further invites either worker members who have been trained by the WHSC to develop and deliver the supervisor training, or the PSHSA to deliver the training (Section 9 (20) (21))
Now What?
EUREKA! This matter has been resolved by the IRS!
The foregoing are composite scenarios loosely crafted from actual experiences reported by ONA members. While in some instances, the basic IRS may resolve the safety concerns of our members, too often there is a need to accelerate the IRS and/or call the MLTSD as workplace parties do not work together to establish and maintain safe and healthy work environments. As a result, it is important for ONA members to learn and assert their rights as workers, health and safety representatives and JHSC members, and strengthen their IRS to protect them and their colleagues from harm.
When the IRS breaks down, the Union should not hesitate to call the MLTSD and emphasize the need for a quick response, particularly in a workplace where workers do not have a clear right to refuse unsafe work. If members encounter difficulties, the Bargaining Unit/Labour Relations Officer should be contacted for advice.
Ministry of Labour
Ministère du Travail
Healthcare, Strategy Unit
505 University Avenue, 2nd Floor
Toronto, ON M7A 1T7
Tel: (416) 326-2913
Fax: (416) 326-2988
Ms. Erna Bujna
Labour Relations Specialist
Workers Compensation/Occupational Health and Safety
Ontario Nurses’ Association
85 Grenville Street, Suite 400
Toronto, ON
M5S 3A2
Dear Ms. Bujna:
Thank you for your electronic mail correspondence dated December 6 and 12, 2007 regarding the legislated requirements to notify the Joint Health and Safety Committee (JHSC) and trade unions of workplace injuries.
For workplaces covered by:
- Section 2 of the Health Care and Residential Facilities Regulation (O Reg. 67/93), or
- The Regulations for Industrial Establishments 851/90 (industrial establishments as defined in the Occupational Health and Safety Act, RSO 1990, Chapter O.1
The employer is obligated to notify the JHSC and trade union of workplace injuries and occupational illnesses as required by sections 51 (1) and 52 of the Occupational Health and Safety Act and section 5(2) and 5(3) of both the Health Care and Residential Facilities Regulations for Industrial Establishments.
ONA Question 1: “If it is the MOL position that the employer is obligated to provide to the JHSC and the trade union written notice within 4 days of the occurrence containing the prescribed information and particulars (s. 5 hc and industrial regs)”
Ministry of Labour (MOL) response: Yes, for an accident (see the Occupational Health and Safety Act, section 52 (1)) and an occupational illness (see the Occupational Health and Safety Act, section 52(2)). The employer is required to provide the information and particulars prescribed by the regulations in order to meet the statutory requirements.
ONA Question 2: “Does the MOL in any way agree that an employer has met compliance by only providing a monthly summary of all accidents and illness to the JHSC?”
MOL response: This would not comply with the requirements of sections 51 and 52 of the Occupational Health and Safety Act.
ONA Question 3: “Is there any type of memo to all Directors/Inspectors that the MOL would be prepared to issue to its inspectors and Directors to reinforce the employers complete obligations under Section 51, 52 and Section 5 of the health care regulation and reminding inspectors to check with the JHSC worker members and the unions to see how they receive accident information from the employer and where the employer is in violation, asking inspectors to write orders/prosecute?”
MOL response: The Ministry of Labour has advised healthcare inspectors during training programs and on other occasions of the requirements, most recently at a meeting on December 12, 2007.
Ministry of Labour inspectors routinely audit functioning of the internal responsibility system (IRS) during workplace inspections. Components of this include accident notification and JHSC functioning. Enforcement tools to ensure compliance with the Act and related regulations include issuing of orders.
Your e-mail of December 12, 2007 references a Ministry of Labour inspection xxxxxxxxx
Nancy Johnson’s e-mail of December 14, 2007 references the xxxxxxxx You must discuss these workplace specific concerns directly with the inspectors’ manager or the appropriate Regional Director for resolution. Please remind your members that if there are unresolved concerns at specific workplaces, these should be referred to the closest Ministry of Labour Regional Office.
The material in this e-mail is being provided as information only. Reference should always be made to the Occupational Health and Safety Act and the regulations to ascertain one’s rights and duties under the law. It is the responsibility of all workplace parties to ensure compliance with the Occupational Health and Safety Act and the regulations and to seek independent legal advice where questions remain.
Thank you for your correspondence.
Sincerely,
“Leon Genesove” MD DIH FCBOM FRCPC
Provincial Physician
Team Lead, Healthcare Team
Occupational Health and Safety Branch
CC: Carol Sackville-Duyvelsholf, (A) Director, OHSB
Eve McDonald
Appendix B: Sample Template – Hazards and Recommendations to Employer
This is only a sample template designed to help ease the job of an ONA JHSC member. Section 9 (18-21) of the OHSA does not specify the form of a recommendation written by a JHSC or co-chair. To trigger a written response from an employer within 21 days, it is only required that the JHSC or co-chair recommendation be in written form. Legally, you can use this template, a letter, email or any written form to submit recommendations to the employer. Regardless of the form of the recommendation, it is important to note the date sent, the hazard/concern identified and/or the recommendation that the JHSC or co-chair is proposing. It helps to number each hazard/concern. Attempt to secure JHSC consensus and have both co-chairs sign the recommendations. If consensus cannot be reached, the co-chair may submit the recommendation(s) independently.
Date:____________________________
Hand delivered to: __________________________
(Insert name of Employer)
(Insert address of Employer)
Pursuant to Section 9 (18) of the Occupational Health and Safety Act, (OHSA) among our functions as a Joint Health and Safety Committee (JHSC) we are to:
- “identify situations that may be a source of danger or hazard to workers
- make recommendations to the employer and the workers for the improvement of their health and safety
- recommend to the employer and the workers the establishment, maintenance and monitoring of programs, measures and procedures respecting the health and safety of workers, and the trade union representing the workers.”
As such, we or I (if no consensus reached by JHSC then worker co-chair should replace “we” with “I”) have identified the following source(s) of danger or hazard, and/or concern(s), at [insert address of employer] and/or provide the following recommendations:
Identified Hazards or Dangers and/or concerns and their associated Recommendations
| Hazard/Concern | Recommendations |
|---|---|
| Risk posed by supervisors who are not “competent” as defined in the OHSA. Permanent supervisors, workers who may have “charge of a workplace or authority over a worker”, are not trained in the OHSA and how it applies to the work. They are not trained to identify hazards or in how to take every precaution reasonable to protect workers. | The employer to identify all appointed supervisors as defined in the OHSA and demonstrate how it will ensure that all supervisors are “competent” as defined in the OHSA.
As a minimum they should receive and be able to demonstrate their knowledge of:
|
If the committee has failed to reach consensus about making recommendations under section 9 Subsection (18) of the OHSA after attempting in good faith to do so, either co-chair of the committee has the power to make written recommendations to the constructor or employer.
Pursuant to S. 9 (20), an employer who receives written recommendation(s) from a committee or co-chair shall respond in writing within 21 days. Therefore, we look forward to receiving your written response to our recommendations within 21 days, i.e., by [enter date].
We anticipate that your written response will include all information pursuant to the OHSA Section 9 (21), which says: “A response of a constructor or employer under Subsection (20) shall contain a timetable for implementing the recommendations the constructor or employer agrees with and give reasons why the constructor or employer disagrees with any recommendations that the constructor or employer does not accept.”
Please sign below.
____________________________, Worker Co-Chair, Joint Health and Safety Committee
____________________________, Employer Co-Chair, Joint Health and Safety Committee
C: Post for the workers
Copy to JHSC
Bargaining Unit President
APPENDIX C: Sample Letter to Directors and Officers of Corporation
XXXXX, 20XX
Board of Directors
CEO
XXX Hospital
XXX
XXX, ON A1C D2F
Dear XXX,
Our unions have grave concerns about the state of occupational health and safety at XXX Hospital. We are frustrated that after years of effort, there is still no real health and safety culture at the hospital, and adequate systems are not in place to protect workers from illness and injury. This situation is completely unacceptable. We point you to the findings of the comprehensive three-year investigation by the Ontario SARS Commission of Inquiry. Commissioner Justice Archie Campbell found:
“Hospitals are dangerous workplaces, like mines and factories, yet they lack the basic health and safety culture and workplace safety systems that have become expected and accepted for many years in Ontario mines and factories and in British Columbia’s hospitals.”
Justice Campbell counseled hospitals to “listen more carefully” to the health and safety concerns and advice of unions and front-line workers. At XXX Hospital, despite several years of well- documented efforts, many of our concerns have been minimized or dismissed, and we have not seen significant improvements in our workplace. The state of XXX Hospital’s health and safety is disquieting enough, but our concern is heightened by the knowledge that we are facing major construction and all of the additional potential hazards associated with such an enterprise. We feel a pressing need to inform the highest levels of the hospital of our concerns, reasons for them, and of the need for your prompt and substantial attention to this problem.
The centerpiece of any effective health and safety culture is a concept known as the Internal Responsibility System (IRS), which is the implicit framework of Ontario’s Occupational Health and Safety Act (OHSA). There can be no IRS until the employer first complies with its legislated responsibilities to establish occupational health and safety policies, programs, measures, procedures, equipment and training. The employer must then ensure that supervisors are knowledgeable about legislation and hazards, and respond to and resolve health and safety concerns. The employer must also ensure that workers are trained about legislation, hazards and how to work safely. The employer must establish, and facilitate the activities of a Joint Health and Safety Committee (JHSC), which monitors and provides advice about workplace health and safety.
In our experience, XXX Hospital management talks a lot about an IRS, but has not done enough to establish one. For example:
- Fumes from XXX in XXX made workers ill and necessitated the evacuation of patients from one floor of the hospital. Several air quality incidents were reported in that time period, XXXXXX.Now almost X years later, there is still no clear system for handling complaints and preventing injury, this despite the fact that there have been several incidents in the intervening years. In XXX, the employer’s solution to persistent hazards was to suggest that the lead union activist in this area be reassigned. XXXXXX.More recently, there was yet another incident on XXX and some of our members contacted the MLTSD to investigate.In response at the next JHSC meeting, the employer co-chair criticized workers for contacting the MOL.Worker members were disturbed by the employer’s intimidating response. Instead of learning lessons from the incident and taking steps to prevent similar hazards in future, the employer tried to suppress the issue and intimidate workers for seeking enforcement of the OHSA. We fear such a response does not bode well for the increasing hazards our members will surely face when hospital construction resumes.In fact, even more recently, on XXX, there was yet another XXX incident in the same area. This time, XXX called the MLTSD with a formal union complaint and a XXX order was issued.
- The employer has not been complying with its legislated responsibility to notify the JHSC and unions of injuries. Furthermore, for several months, management recently produced a disturbing report about incidents and injuries, which clearly illustrates an upward trend in first aid, lost time and recurrent injuries.
- Training of supervisors in occupational health and safety legislation and hazards is not only required by legislation, it is key to building a solid Our unions have long been asking the employer to ensure supervisor “competency” (defined under the OHSA), but have seen no evidence of progress. As illustrated in point #1 above (and countless other examples), supervisors continue to exhibit inattention to worker health and safety and appalling ignorance of their own personal legislated responsibilities and liabilities.
- Despite specific funding from the Ministry of Health and Long-term Care (MOHLTC), progress in implementing safety engineered medical devices to prevent needlestick injuries has been slow. Training is deficient and we have recently had another HIV needlestick exposure, with no investigation of this critical injury by the JHSC nor the MLTSD.
- Years ago, the MOHLTC provided funding for the installation of ceiling lifts to protect workers from back injuries, but such equipment must be properly installed and regularly The hospital has not instituted a program of inspection and repair of this equipment, and now there are increasing reports of failure. This is in stark contrast to other Ontario hospitals, which recognized early the need and the requirement to be as respectful of patient lifting equipment as they are of material lifting equipment, instituting at least an annual inspection and refurbishment of all patient lifts by a competent person.
- Over the years, many of our members have been exposed to workplace violence, and across the country similar incidents, with slightly different circumstances, have had horrificYet, XXX Hospital still does not have a violence prevention program in place. In fact, the issue of one nurse who was recently placed at risk in the Emergency Department was dismissed by JHSC management as a “Building Services” matter not appropriate for discussion by the JHSC! The PSHSA offers training in how to develop and establish policies, programs, procedures, measures, equipment and training for this serious and pervasive hazard in hospitals, and the hospital would be well advised to tap this affordable resource to develop its programs in violence prevention and other health and safety hazards.
- Despite the foregoing and numerous other health and safety deficiencies, and despite the legislative requirement for the employer to facilitate the operation of the JHSC, management members of the JHSC have expressed and demonstrated that they cannot commit time to the operation and the business of the Most recently, management has shortened meetings of the JHSC of this, XX large XX health care facility XXX, to two hours, with only five minutes permitted for discussion of each item on the agenda. Hospitals less than half the size of XXX have made much more significant commitments of staff and resources to their JHSCs, perhaps because they have independently seen the value of a robust IRS and JHSC, or perhaps because they have been made to see its value via prosecution.
In response to our concerns, your management may point out that the XXXX Hospital has managed to escape directed MLTSD attention in its ongoing “high-risk” facility inspections. It is important that you understand that this MLTSD initiative is driven entirely by WSIB statistics from the past three years, and in this period, we have found reason to seriously question the statistics XXX Hospital has provided to WSIB. We have little confidence in the employer’s WSIB statistics, and our actual experiences, some of which are outlined above, make us question why the hospital is not receiving MLTSD initiative attention.
We are nervous. The statistical picture that your own management has painted points to a serious injury on the horizon, and the upcoming construction, particularly in light of our experience with past construction, makes us even more worried. As concerned partners in this workplace, we find it necessary to raise these issues directly to you, and as officers and directors of the corporation, we know you understand as individuals that you must take active steps to investigate and respond to these matters.
As unions, we want nothing more than for our members to go home safe and healthy after the challenges of a day’s work in the demanding health care sector. We want to work collaboratively with the employer to accomplish this goal. But your management and our members have struggled for too long to establish an effective IRS at the hospital. They need senior commitment, advice and direction, as well as committed occupational health and safety leaders representing the employer on the JHSC and championing health and safety in the workplace.
As you deliberate on this most serious issue, we ask you to consider your legislated responsibilities as officers and directors of the corporation, as well Justice Campbell’s warnings to the government about how it needs to respond to health and safety in the health care sector:
“Ontario … slept through many wake-up calls. Again and again the systemic flaws were pointed out, again and again the very problems that emerged [during SARS] were predicted, again and again the warnings were ignored.
The Ontario government has a clear choice. If it has the necessary political will, it can make the financial investment and the long-term commitment to reform that is required to bring our public health protection against infectious disease up to a reasonable standard. If it lacks the necessary political will, it can tinker with the system, make a token investment, and then wait for the death, sickness, suffering and economic disaster that will come with the next outbreak of disease. The strength of the government’s political will can be measured in the months ahead by its actions and its long-term commitments.”
Sincerely,
President Local
C:
APPENDIX D: Joint Union Letter on Unions Working Together on Health and Safety
APPENDIX E: MOL Memo Confirming Priority Response to Complaints
APPENDIX F: Safe Return to Work Algorithm
Appendix G: Resources
The Ontario Nurses’ Association (ONA)
ONA is dedicated to providing all members with the information and support they need in the important area of occupational health and safety.
Here is a list of what we offer:
- ONA provides support to each Bargaining Unit’s occupational health and safety representative/ONA Joint Health and Safety Committee (JHSC) member when there has been a perceived violation of the Occupational Health and Safety Act. Through Local activities, the Bargaining Unit is the primary provider of occupational health and safety services to membership. That includes ensuring there is a functioning JHSC at the Bargaining Unit level when required by the Act. Resource support is provided to Bargaining Units by the Labour Relations Officers (LROs) of ONA’s four district service teams (North, South, West and East).
- Each district service team has a Labour Relations Officer with the primary responsibility for planning and coordinating the occupational health and safety services provided in ONA’s five However, that does not mean occupational health and safety is the sole function of that Labour Relations Officer. The district service teams deliver occupational health and safety services through a variety of means.
Additionally at the provincial level, support is provided to staff and membership by the Regional Vice-President who holds the portfolio for occupational health and safety. Supporting staff include the Labour Relations Officers who specialize in occupational health and safety, Workplace Safety and Insurance Board Appeals, Professional Practice Specialists, the Human Rights Specialist who can provide guidance and assistance regarding the duty to accommodate under the Ontario Human Right Code, and Long-Term Disability (LTD) Primes who can assist in instances of LTD benefit denials, appeals or reinstatement with employers and insurance carriers.
- ONA’s website (www.ona.org) contains useful information, resources and tools pertaining to many health and safety
Contact Information and listing for our Provincial and Regional Offices may be found at: https://www.ona.org/contact-us/
Workers Health and Safety Centre (WHSC)
The WHSC is one of the Safe Workplace Associations funded by the Ministry of Labour/Workplace Safety and Insurance Board. Based in Ontario, this worker-driven organization’s mandate is to effectively develop and provide occupational health and safety leadership, training and education programs and information services that meet workers’ needs and are consistent with labour’s principles. Their mandate also includes promoting activities that involve workers in health and safety matters and improve working conditions and worker well- being. Its website also contains information on training programs and a service allowing you to ask health and safety-related questions.
WHSC Head Office
675 Cochrane Dr., Suite 710, East Tower Markham, ON L3R 0B8
Tel: 416-441-1939
Toll free: 1-888-869-7950 Website: www.whsc.on.ca
WHSC Regional Offices can be reached toll free at 1-888-869-7950. Their regional office locations are also available on their website.
Public Services Health and Safety Association (PSHSA)
The Public Services Health and Safety Association (PSHSA) is a not-for-profit organization, designated as a Safe Workplace Association (SWA) under the Workplace Safety and Insurance Act (S.O. 1997) funded by the Ministry of Labour. The mandate of PSHSA is to educate and guide their health care and community services clients to proactively adopt occupational health and safety best practices and strategies that will prevent workplace fatalities, injuries, and illnesses.
PSHSA Head Office
4950 Yonge Street, Suite 1800 Toronto, ON M2N 6K1
Tel: (416) 250-2131
Fax: (416) 250-7484
Toll-free: 1-877-250-7444
Website: www.pshsa.ca
Occupational Health Clinic for Ontario Workers (OHCOW)
The Occupational Health Clinic for Ontario Workers (OHCOW) is a non-profit organization. It is one of the Health and Safety Associations funded by the Ministry of Labour/Workplace Safety and Insurance Board.
The mission of OHCOW is to prevent occupational illnesses and injury, and to promote the highest degree of physical, mental and social well-being of all workers.
OHCOW strives to accomplish this through the identification of workplace factors which are detrimental to the health and well-being of all workers, through the distribution of excellent occupational health, hygiene, and ergonomic information to increase knowledge among workers, employers and the general public; and through the provision of services designed to produce changes to improve workplaces and the health of workers.
Staffed by an inter-disciplinary team of doctors, nurses, hygienists, ergonomists, researchers and administrators, each OHCOW clinic provides comprehensive occupational health services and information in five areas:
- An inquiry service to answer work-related health and safety
- Medical diagnostic services for workers who may have work-related health
- Group prevention service for workplace health and safety committees and groups of workers.
- Outreach and education to increase awareness of health and safety issues and promote prevention
- Research services to investigate and report on illnesses and
- The clinic’s services are free of charge to workplace
OHCOW Provincial Office
1090 Don Mills Road, Suite 606 Toronto, ON, M3C 3R6
Tel: (416) 510.8713
Fax: (416) 443.9132
E-mail: info@ohcow.on.ca Website: www.ohcow.on.ca
All clinics can be reached toll free at 1-877-817-0336. All locations of their regional offices are listed on their website.
Criminal Injuries Compensation Board
The Criminal Injuries Compensation Board can award compensation to victims of crimes of violence occurring in Ontario.
Head Office
655 Bay Street, 14th Floor
Toronto, ON M7A 2A3
Tel: (416) 326-2900
Toll-free: 1-800-372-7463
Fax: (416) 326-2883
Website: www.sjto.gov.on.ca/cicb
Canadian Centre for Occupational Health and Safety
The Canadian Centre for Occupational Health and Safety (CCOHS) promotes a safe and healthy working environment by providing information and advice about occupational health and safety.
CCOHS fulfills its mandate to promote workplace health and safety and encourage attitudes and methods that will lead to improved worker physical and mental health through a wide range of products and services. These products and services are designed in cooperation with national and international occupational health and safety organizations, with an emphasis on preventing illnesses, injuries and fatalities. They provide a variety of both public service initiatives at no charge to the user, such as OSH Answers, the person-to-person Inquiry Service, an electronic newsletter and public presentations. Services for specialty resources provided on a cost-recovery basis include database subscriptions, manuals and training programs.
CCOHS Head Office
135 Hunter Street East
Hamilton, ON L8N 1M5
Tel: (905) 572-2981
Fax: (905) 572-2206
Website: www.ccohs.ca
Inquiries and Client Services
The CCOHS Inquiries and Client Services Team is dedicated to answering any questions you may have, whether it be a health or safety concern about the work you do, or about its many products and services. This person-to-person service is offered via web, phone or fax.
Tel: (905) 570-8094
Toll-free: 1-800-668-4284
Fax: (905) 572-4500
Website: www.ccohs.ca (on-line form)
The National Institute for Occupational Safety and Health
The American National Institute for Occupational Safety and Health (NIOSH) is the federal agency responsible for conducting research and making recommendations for the prevention of work- related injury and illness. NIOSH is part of the Centers for Disease Control and Prevention (CDC) in the Department of Health and Human Services.
NIOSH is in the U.S. Department of Health and Human Services and is an agency established to help ensure safe and healthful working conditions for working men and women by providing research, information, education and training in the field of occupational safety and health.
NIOSH provides national and world leadership to prevent work-related illness, injury, disability and death by gathering information, conducting scientific research and translating the knowledge gained into products and services. NIOSH’s mission is critical to the health and safety of every American worker.
The NIOSH website provides access to the full range of NIOSH information and publications.
CDC/NIOSH Contact Information
1-800-CDC-INFO (1-800-232-4636)
TTY: 1-888-232-6348
Fax: 1-513-533-8347
E-mail: cdcinfo@cdc.gov
Website: www.cdc.gov
Ontario Ministry of Labour, Training and Skills Development
Established in 1919 to develop and enforce labour legislation, the mission of the MLTSD is to advance safe, fair and harmonious workplace practices that are essential to the social and economic well-being of the people of Ontario. As of April 2012, prevention resources have been moved from the WSIB to a newly formed Chief Prevention Office in the MLTSD.
Through the Ministry’s key areas of occupational health and safety, employment rights and responsibilities, labour relations and internal administration, the Ministry’s mandate is to set, communicate and enforce workplace standards while encouraging greater workplace self-reliance. A range of specialized agencies, boards and commissions assist the Ministry in its work. The MLTSD inspectors are who you call for unresolved health and safety issues. They have the ability to write orders that employers must comply with.
MLTSD Main Office – Toronto Occupational Health and Safety Branch
400 University Avenue,14th Floor
Toronto ON M7A 1T7
Toll Free: 1-877-202-0008
TTY: 1-855-653-9260
Fax: (905) 577-1316
Website: www.labour.gov.on.ca
All locations of their regional offices are listed on their website.
Contacting the MLTSD
To make a complaint, report critical injuries, fatalities, work refusals or other concerns at any time of day, please call the Ministry of Labour Health and Safety Contact Centre’s toll-free number, 1-877-202-0008.
Complaints can also be made online by going to the MLTSD website listed above, and choosing “File a Complaint”.
You can also email your questions to webohs@ontario.ca.
Employers should send notice of an occupational illness as well as any written reports of fatalities or critical injuries to the attention of the Director at their regional MLTSD Office. This contact information can be found on their website. Reports of occupational exposures can also be sent to MLTSDoccillness.notices@ontario.ca.
APPENDIX H: Unresolved Health and Safety Concerns: Guidelines re: When to Call the Ministry of Labour, Training and Skills Development
Action: Workers must report health and safety hazards/concerns to their supervisors. The JHSC and Union should raise unresolved health and safety concerns as high as necessary and as quickly as necessary to make workers safe
Introduction
Among their functions, MLTSD inspectors are expected to investigate:
- Internal Responsibility System (IRS) failures and other complaints.
- Critical and fatal injuries/illnesses.
- Work refusals/work stoppages.
When the inspector finds sufficient evidence, they can enforce the law by issuing orders and/or laying charges under the Occupational Health and Safety Act (OHSA).
This document is designed to assist ONA members with deciding when it is appropriate to call the MLTSD for help in their workplace.
Who Can Call the Ministry of Labour Training, Skills and Development?
Anyone can call the Ministry of Labour to seek enforcement of the OHSA or the regulations. The JHSC and Union should contact the MOL when hazards remain unresolved or pose imminent danger to a worker.
When Should the MLTSD be Called?
- When the IRS fails to resolve concerns
Employers, supervisors, workers, Joint Health and Safety Committee (JHSC) members and others must perform their duties as expressed in the OHSA, and may exercise the rights that are outlined. The government established this legal system of “internal responsibility” in hopes that workplace parties would work together to achieve safe and healthy workplaces without formal intervention (see below for diagram of IRS).ONA recommends that wherever possible, use the IRS. But don’t let issues drag on. When:
-
- exposure to a serious hazard is imminent or
- there is prolonged potential or actual exposure to a hazard due to the failure or the sluggishness of the IRS,
- Report your concern to your If unresolved, the JHSC and Union should raise the issue with the employer as high as necessary (e.g., JHSC, director, CEO, Board of Directors) and as quickly as necessary (e.g. phone, e-mail, in person) to protect a worker.
- Work with your Labour Relations Officer, who will assist in raising the issue within the union as high as necessary and as quickly as necessary to protect a worker (e.g., JHSC, Local Coordinator, specialists, manager, ONA Leadership, Board of Directors, Communications and Government Relations Team).
- Consider grieving where appropriate/available, but don’t just rely on the grievance process to save someone from injury/illness. Use the law and the MLTSD.
When internal workplace efforts to resolve a health and safety concern fail, the JHSC and the Union should call the MLTSD.
- Consider grieving where appropriate/available, but don’t just rely on the grievance process to save someone from injury/illness. Use the law and the MLTSD.
- When an employer fails to notify the MLTSD of a fatal or critical injury and/or does not permit the JHSC to investigate
The employer is required by sections 51-53 of the OHSA to report critical and fatal injuries to the MLTSD, the union and the JHSC, and section 9 empowers the JHSC to investigate. When an employer does not comply with these sections, the JHSC and the Union should call the MLTSD. - When work refusal reaches “second stage”
When a worker exercises their right to refuse unsafe work, the supervisor or employer must immediately investigate in the presence of the worker and a JHSC worker member. (OHSA section 43). If the concern is not resolved and the worker has reasonable grounds to believe that the work continues to be unsafe, the worker can continue to refuse. At this “second stage” of the refusal, the MLTSD must be notified. - When bilateral work stoppage is not resolved
A certified JHSC member who has reason to believe that “dangerous circumstances” (defined in OHSA section 44) exist may request an investigation by a supervisor, and thereafter by a second certified member. If the investigations do not resolve the concern, the MLTSD must be notified.
How to Make Your Call to the MLTSD Effective
Be aware that MLTSD intake officers often ask a caller if they have exhausted the IRS before calling the MLTSD.
If the caller answers in the negative, some of these officers have been known to refuse to pass on the information or send an inspector. ONA has convinced upper levels of the MLTSD that the IRS is generally not working in health care facilities and that we need the assistance of the MLTSD to prod employers to comply with their legal duty to establish functioning Internal Responsibility Systems. If necessary, remind the MLTSD that because our members have a limited right to refuse unsafe work, and the only thing between them and imminent jeopardy may be the MLTSD, the Ministry long ago committed to responding to our members’ complaints on a “priority complaint basis” (see memo at Appendix E).
Also, the IRS is implicit in the Occupational Health and Safety Act. While it is the preferred process of resolving health and safety concerns, anyone can call the Ministry of Labour to seek enforcement of the OHSA or the regulations. The JHSC and Union should contact the MLTSD when hazards remain unresolved or pose imminent danger to a worker.
For a listing of MLTSD contact information, see Appendix G.
Worker to Suffer no Reprisals for Calling the MLTSD
The Occupational Health and Safety Act has a section (50) that is intended to protect you from reprisals by your employer when you obey the law or exercise your rights. The Ministry of Labour website says you also cannot be penalized if you provide information to a MLTSD inspector, follow an order of an inspector, or testify in a legal proceeding. If you think you or your members have suffered a reprisal, you or your members can file a complaint to the Ontario Labour Relations Board (OLRB) or file a grievance. The employer has the onus to prove that they did not act illegally.
Unsatisfactory MLTSD Decision
When not satisfied with an inspector’s decision, work with your Labour Relations Officer, who will assist in the union’s efforts to raise the issue within the MLTSD/ government as high as necessary and as quickly as necessary to protect a worker (e.g., MLTSD manager, director, Assistant Deputy Minister, Deputy Minister, Premier)
o With your Labour Relations Officer, consider appeal of inspector decisions (30-day time limit) as appropriate.
Appendix I: Ten Operating Principles for Guiding Effective Participation
From the survey and stories, we started to see similarities in the elements that made knowledge activist representatives more effective and successful. We were able to summarize them:
- Research: Strategically conduct and use research to make claims, present solutions, and build legitimacy and trust.
- More than just meetings: Emphasize the importance of working with and outside committees. Effective representation requires an activist approach.
- Mobilize your influence: Recognize and understand the challenges and consequences of representation. Know how to mobilize influence using knowledge, the law and worker support. Be prepared for push back from some in management.
- Listen to workers: Making change requires listening to and acknowledging concerns of other workers. Build from their experience and engage them with education that is needed. Train co-workers in health and safety. Engage them in the monitoring and change process.
- Address authority: Understand that influencing management requires an ongoing effort to educate and influence their way of seeing things (e.g., constantly reinforce messages like health and safety pays).
- Build trust: Recognize the importance of building relationships in the committee and in the workplace and build trust, mutual respect and legitimacy.
- Be assertive: Be assertive, persistent and keep your cool. Be diplomatic. Figure out how to move forward over the long term if there is resistance. If you draw a bottom line, have a strategy to defend that bottom line.
- Build solutions: Don’t just identify the problem. Provide and work with management to develop solutions that address the source of the hazard.
- Use inspections and minutes: Recognize the value of inspections, reports and minutes but do not define your role just in these terms. Beware management efforts to confine your activities to a technocratic or bureaucratic box (i.e., keeping reps busy with reports, imposing long drawn-out processes for decision-making, responding to numerous minor issues and limiting access to shopfloor or workers).
- Use the law strategically: Recognize the limitations of the law but know and use the law and regulations where they provide leverage. Develop a relationship of trust with local MLTSD inspectors and use that relationship tactically and strategically.
APPENDIX J: Form for Reporting an Unresolved Health and Safety Hazard to Supervisor
TO: (“supervisor” as defined in section 1 of the Occupational Health and Safety Act (OHSA)
Pursuant to my legal duty under section 28 of the OHSA, on I reported a health and safety hazard to you. The hazard has not been addressed.
The concern is:
XXX
The OHSA requires the employer (section 25 (2) (h)) and the supervisor (section 27 (2) (c)) to take every precaution reasonable in the circumstances to protect a worker.
Signed
Date
C. Bargaining Unit President JHSC members